What Are the Most Common Shoulder Problems?
The most movable joint in the body, the shoulder is also one of the most potentially unstable joints. As a result, it is the site of many common problems. They include sprains, strains, dislocations, separations, tendinitis, bursitis, torn rotator cuffs, frozen shoulder, fractures, and arthritis. Specific shoulder problems will be discussed later in this publication.
- How Common Are Shoulder Problems?
- What Are the Structures of the Shoulder and How Does It Function?
- What Are the Origins and Causes of Shoulder Problems?
- How Are Shoulder Problems Diagnosed?
- What Should I Know About Specific Shoulder Problems, Including Their Symptoms and Treatment?
- What Research Is Being Conducted on Shoulder Problems?
- Where Can People Find More Information About Shoulder Problems?
- Key Words
Illustration
Information Box
How Common Are Shoulder Problems?
According to the Centers for Disease Control and Prevention, nearly 1.2 million people in the United States visited an emergency room in 2010 for shoulder problems.
1Centers for Disease Control and Prevention (CDC)/National Center for Health Statistics (NCHS), National Hospital Ambulatory Medical Care Survey. National Hospital Ambulatory Medical Care Survey: 2010 Emergency Department Summary Tables. Accessed April 10, 2014, at http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2010_ed_web_tables.pdf.
What Are the Structures of the Shoulder and How Does It Function?
To better understand shoulder problems and how they occur, it helps to begin with an explanation of the shoulder’s structure and how it functions.
The shoulder joint is composed of three bones: the clavicle (collarbone), the scapula (shoulder blade), and the humerus (upper arm bone) (see illustration). Two joints facilitate shoulder movement. The acromioclavicular (ah-KRO-me-o-klah-VIK-u-lahr or AC) joint is located between the acromion (ah-KRO-me-on, the part of the scapula that forms the highest point of the shoulder) and the clavicle. The glenohumeral joint, commonly called the shoulder joint, is a ball-and-socket-type joint that helps move the shoulder forward and backward and allows the arm to rotate in a circular fashion or hinge out and up away from the body. (The “ball,” or humerus, is the top, rounded portion of the upper arm bone; the “socket,” or glenoid, is a dish-shaped part of the outer edge of the scapula into which the ball fits.) The capsule is a soft tissue envelope that encircles the glenohumeral joint. It is lined by a thin, smooth synovial membrane.
Structure of the Shoulder

In contrast to the hip joint, which more closely approximates a true ball-and-socket joint, the shoulder joint can be compared to a golf ball and tee, in which the ball can easily slip off the flat tee. Because the bones provide little inherent stability to the shoulder joint, it is highly dependent on surrounding soft tissues such as capsule ligaments and the muscles surrounding the rotator cuff to hold the ball in place. Whereas the hip joint is inherently quite stable because of the encircling bony anatomy, it also is relatively immobile. The shoulder, on the other hand, is relatively unstable but highly mobile, allowing an individual to place the hand in numerous positions. It is, in fact, one of the most mobile joints in the human body.
The bones of the shoulder are held in place by muscles, tendons, and ligaments. Tendons are tough cords of tissue that attach the shoulder muscles to bone and assist the muscles in moving the shoulder. Ligaments attach shoulder bones to each other, providing stability. For example, the front of the joint capsule is anchored by three glenohumeral ligaments. The rotator cuff is a structure composed of tendons that work along with associated muscles to hold the ball at the top of the humerus in the glenoid socket and provide mobility and strength to the shoulder joint. Two filmy sac-like structures called bursae permit smooth gliding between bones, muscles, and tendons. They cushion and protect the rotator cuff from the bony arch of the acromion.
What Are the Origins and Causes of Shoulder Problems?
The shoulder is easily injured because the ball of the upper arm is larger than the shoulder socket that holds it. To remain stable, the shoulder must be anchored by its muscles, tendons, and ligaments.
Although the shoulder is easily injured during sporting activities and manual labor, the primary source of shoulder problems appears to be the natural age-related degeneration of the surrounding soft tissues such as those found in the rotator cuff. The incidence of rotator cuff problems rises dramatically as a function of age and is generally seen among individuals who are more than 60 years old. Often, the dominant and nondominant arm will be affected to a similar degree. Overuse of the shoulder can lead to more rapid age-related deterioration.
Shoulder pain may be localized or may be felt in areas around the shoulder or down the arm. Disease within the body (such as gallbladder, liver, or heart disease, or disease of the cervical spine of the neck) also may generate pain that travels along nerves to the shoulder. However, these other causes of shoulder pain are beyond the scope of this publication, which will focus on problems within the shoulder itself.
How Are Shoulder Problems Diagnosed?
As with any medical issue, a shoulder problem is generally diagnosed using a three-part process.
- Medical history. The patient tells the doctor about any injury or other condition that might be causing the pain.
- Physical examination. The doctor examines the patient to feel for injury and to discover the limits of movement, location of pain, and extent of joint instability.
- Tests. The doctor may order one or more of the tests listed below to make a specific diagnosis. These tests may include the following.
- Standard x ray. A familiar procedure in which low-level radiation is passed through the body to produce a picture called a radiograph. An x ray is useful for diagnosing fractures or other problems of the bones. Soft tissues, such as muscles and tendons, do not show up on x rays.
- Arthrogram. A diagnostic record that can be seen on an x ray after injection of a contrast fluid into the shoulder joint to outline structures such as the rotator cuff. In disease or injury, this contrast fluid may either leak into an area where it does not belong, indicating a tear or opening, or be blocked from entering an area where there normally is an opening.
- Ultrasound. A noninvasive, patient-friendly procedure in which a small, hand-held scanner is placed on the skin of the shoulder. Just as ultrasound waves can be used to visualize the fetus during pregnancy, they can also be reflected off the rotator cuff and other structures to form a high-quality image of them. The accuracy of ultrasound for the rotator cuff is particularly high.
- MRI (magnetic resonance imaging). A noninvasive procedure in which a machine with a strong magnet passes a force through the body to produce a series of cross-sectional images of the shoulder.
Other diagnostic tests, such as one that involves injecting an anesthetic into and around the shoulder joint, are discussed in detail in other parts of this publication.
What Should I Know About Specific Shoulder Problems, Including Their Symptoms and Treatment?
The symptoms of shoulder problems, as well as their diagnosis and treatment, vary widely, depending on the specific problem. The following is important information to know about some of the most common shoulder problems.
Dislocation
The shoulder joint is the most frequently dislocated major joint of the body. In a typical case of a dislocated shoulder, either a strong force pulls the shoulder outward (abduction) or extreme rotation of the joint pops the ball of the humerus out of the shoulder socket. Dislocation commonly occurs when there is a backward pull on the arm that either catches the muscles unprepared to resist or overwhelms the muscles. When a shoulder dislocates frequently, the condition is referred to as shoulder instability. A partial dislocation in which the upper arm bone is partially in and partially out of the socket is called a subluxation.
- Signs and symptoms. The shoulder can dislocate either forward, backward, or downward. When the shoulder dislocates, the arm appears out of position. Other symptoms include pain, which may be worsened by muscle spasms, swelling, numbness, weakness, and bruising. Problems seen with a dislocated shoulder are tearing of the ligaments or tendons reinforcing the joint capsule and, less commonly, bone and/or nerve damage.
- Diagnosis. Doctors usually diagnose a dislocation by a physical examination; x rays may be taken to confirm the diagnosis and to rule out a related fracture.
- Treatment. Doctors treat a dislocation by putting the ball of the humerus back into the joint socket, a procedure called a closed reduction. The arm is then stabilized for several weeks in a sling or a device called a shoulder immobilizer. Usually the doctor recommends resting the shoulder and applying ice three or four times a day. After pain and swelling have been controlled, the patient enters a rehabilitation program that includes exercises. The goal is to restore the range of motion of the shoulder, strengthen the muscles, and prevent future dislocations. These exercises may progress from simple motion to the use of weights.
After treatment and recovery, a previously dislocated shoulder may remain more susceptible to reinjury, especially in young, active individuals. Ligaments may have been stretched or torn, and the shoulder may tend to dislocate again. A shoulder that dislocates severely or often, injuring surrounding tissues or nerves, usually requires surgical repair to tighten stretched ligaments or reattach torn ones.
Sometimes the doctor performs surgery through a tiny incision into which a small scope (arthroscope) is inserted to observe the inside of the joint. After this procedure, called arthroscopic surgery, the shoulder is generally stabilized for about 6 weeks. Full recovery takes several months. In other cases, the doctor may repair the dislocation using a traditional open surgery approach.
Separation
A shoulder separation occurs where the collarbone (clavicle) meets the shoulder blade (scapula). When ligaments that hold the joint together are partially or completely torn, the outer end of the clavicle may slip out of place, preventing it from properly meeting the scapula. Most often, the injury is caused by a blow to the shoulder or by falling on an outstretched hand.
- Signs and symptoms. Shoulder pain or tenderness and, occasionally, a bump in the middle of the top of the shoulder (over the acromioclavicular or AC joint) are signs that a separation may have occurred.
- Diagnosis. Doctors may diagnose a separation by performing a physical examination. They may confirm the diagnosis and determine the severity of the separation by taking an x ray. While the x ray is being taken, the patient makes the separation more pronounced by holding a light weight that pulls on the muscles.
- Treatment. A shoulder separation is usually treated conservatively by rest and wearing a sling. Soon after injury, an ice bag may be applied to relieve pain and swelling. After a period of rest, a therapist helps the patient perform exercises that put the shoulder through its range of motion. Most shoulder separations heal within 2 or 3 months without further intervention. However, if ligaments are severely torn, surgical repair may be required to hold the clavicle in place. A doctor may wait to see if conservative treatment works before deciding whether surgery is required.
Rotator Cuff Disease: Tendinitis and Bursitis
These conditions are closely related and may occur alone or in combination.
Tendinitis is inflammation (redness, soreness, and swelling) of a tendon. In tendinitis of the shoulder, the rotator cuff and/or biceps tendon become inflamed, usually as a result of being pinched by surrounding structures. The injury may vary from mild inflammation to involvement of most of the rotator cuff. When the rotator cuff tendon becomes inflamed and thickened, it may get trapped under the acromion. Squeezing of the rotator cuff is called impingement syndrome.
Bursitis, or inflammation of the bursa sacs that protect the shoulder, may accompany tendinitis and impingement syndrome. Inflammation caused by a disease such as rheumatoid arthritis may cause rotator cuff tendinitis and bursitis. Sports involving overuse of the shoulder and occupations requiring frequent overhead reaching are other potential causes of irritation to the rotator cuff or bursa and may lead to inflammation and impingement.
If the rotator cuff and bursa are irritated, inflamed, and swollen, they may become squeezed between the head of the humerus and the acromion. Repeated motion involving the arms, or the effects of the aging process on shoulder movement over many years, may also irritate and wear down the tendons, muscles, and surrounding structures.
- Signs and symptoms. Signs of these conditions include the slow onset of discomfort and pain in the upper shoulder or upper third of the arm and/or difficulty sleeping on the shoulder. Tendinitis and bursitis also cause pain when the arm is lifted away from the body or overhead. If tendinitis involves the biceps tendon (the tendon located in front of the shoulder that helps bend the elbow and turn the forearm), pain will occur in the front or side of the shoulder and may travel down to the elbow and forearm. Pain may also occur when the arm is forcefully pushed upward overhead.
- Diagnosis. Diagnosis of tendinitis and bursitis begins with a medical history and physical examination. X rays do not show tendons or the bursae, but may be helpful in ruling out bony abnormalities or arthritis. The doctor may remove and test fluid from the inflamed area to rule out infection. Impingement syndrome may be confirmed when injection of a small amount of anesthetic (lidocaine hydrochloride) into the space under the acromion relieves pain.
- Treatment. The first step in treating these conditions is to reduce pain and inflammation with rest, ice, and anti-inflammatory medicines such as aspirin and ibuprofen (Advil,2 Motrin3). In some cases, the doctor or therapist will use ultrasound (gentle sound-wave vibrations) to warm deep tissues and improve blood flow. Gentle stretching and strengthening exercises are added gradually. These may be preceded or followed by use of an ice pack. If there is no improvement, the doctor may inject a corticosteroid medicine into the space under the acromion. Although steroid injections are a common treatment, they must be used with caution because they may lead to tendon rupture. If there is still no improvement after 6 to 12 months, the doctor may recommend either arthroscopic or open surgery to repair damage and relieve pressure on the tendons and bursae.
2 Brand names included in this publication are provided as examples only, and their inclusion does not mean that these products are endorsed by the National Institutes of Health or any other Government agency. Also, if a particular brand name is not mentioned, this does not mean or imply that the product is unsatisfactory.
3All medicines can have side effects. Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
Torn Rotator Cuff
Rotator cuff tendons often become inflamed from overuse, aging, or a fall on an outstretched hand or another traumatic cause. Sports or occupations requiring repetitive overhead motion or heavy lifting can also place a significant strain on rotator cuff muscles and tendons. Over time, as a function of aging, tendons become weaker and degenerate. Eventually, this degeneration can lead to complete tears of both muscles and tendons. These tears are surprisingly common. In fact, a tear of the rotator cuff is not necessarily an abnormal situation in older individuals if there is no significant pain or disability. Fortunately, these tears do not lead to any pain or disability in most people. However, some individuals can develop very significant pain as a result of these tears and they may require treatment.
- Signs and symptoms. Typically, a person with a rotator cuff injury feels pain over the deltoid muscle at the top and outer side of the shoulder, especially when the arm is raised or extended out from the side of the body. Motions like those involved in getting dressed can be painful. The shoulder may feel weak, especially when trying to lift the arm into a horizontal position. A person may also feel or hear a click or pop when the shoulder is moved. Pain or weakness on outward or inward rotation of the arm may indicate a tear in a rotator cuff tendon. The patient also feels pain when lowering the arm to the side after the shoulder is moved backward and the arm is raised.
- Diagnosis. A doctor may detect weakness but may not be able to determine from a physical examination where the tear is located. X rays, if taken, may appear normal. An MRI or ultrasound can help detect a full tendon tear or a partial tendon tear.
- Treatment. Doctors usually recommend that patients with a rotator cuff injury rest the shoulder, apply heat or cold to the sore area, and take medicine to relieve pain and inflammation. Other treatments might be added, such as electrical stimulation of muscles and nerves, ultrasound, or a cortisone injection near the inflamed area of the rotator cuff. If surgery is not an immediate consideration, exercises are added to the treatment program to build flexibility and strength and restore the shoulder’s function. If there is no improvement with these conservative treatments and functional impairment persists, the doctor may perform arthroscopic or open surgical repair of the torn rotator cuff.
Treatment for a torn rotator cuff usually depends on the severity of the injury, the age and health status of the patient, and the length of time a given patient may have had the condition. Patients with rotator cuff tendinitis or bursitis that does not include a complete tear of the tendon can usually be treated without surgery. Nonsurgical treatments include the use of anti-inflammatory medication and occasional steroid injections into the area of the inflamed rotator cuff, followed by rehabilitative rotator cuff-strengthening exercises. These treatments are best undertaken with the guidance of a health care professional such as a physical therapist, who works in conjunction with the treating physician.
Surgical repair of rotator cuff tears is best for the following individuals.
- Younger patients, especially those with small tears. Surgery leads to a high degree of successful healing and reduces concerns about the tear getting worse over time.
- Individuals whose rotator cuff tears are caused by an acute, severe injury. These people should seek immediate treatment that includes surgical repair of the tendon.
Generally speaking, individuals who are older and have had shoulder pain for a longer period of time can be treated with nonoperative measures even in the presence of a complete rotator cuff tear. These people are often treated similarly to those who have pain but do not have a rotator cuff tear. Again, anti-inflammatory medication, use of steroid injections, and rehabilitative exercises can be very effective. When treated surgically, rotator cuff tears can be repaired by either arthroscopic or traditional open surgical techniques.
Frozen Shoulder (Adhesive Capsulitis)
As the name implies, movement of the shoulder is severely restricted in people with a “frozen shoulder.” This condition, which doctors call adhesive capsulitis, is frequently caused by injury that leads to lack of use due to pain. Rheumatic disease progression and recent shoulder surgery can also cause frozen shoulder. Intermittent periods of use may cause inflammation. Adhesions (abnormal bands of tissue) grow between the joint surfaces, restricting motion. There is also a lack of synovial fluid, which normally lubricates the gap between the arm bone and socket to help the shoulder joint move. It is this restricted space between the capsule and ball of the humerus that distinguishes adhesive capsulitis from a less complicated painful, stiff shoulder. People with diabetes, stroke, lung disease, rheumatoid arthritis, and heart disease, or those who have been in an accident, are at a higher risk for frozen shoulder. People between the ages of 40 and 70 are most likely to experience it.
- Signs and symptoms. With a frozen shoulder, the joint becomes so tight and stiff that it is nearly impossible to carry out simple movements, such as raising the arm. Stiffness and discomfort may worsen at night.
- Diagnosis. A doctor may suspect a frozen shoulder if a physical examination reveals limited shoulder movement. X rays usually appear normal.
- Treatment. Treatment of this disorder focuses on restoring joint movement and reducing shoulder pain. Usually, treatment begins with nonsteroidal anti-inflammatory drugs and the application of heat, followed by gentle stretching exercises. These stretching exercises, which may be performed in the home with the help of a physical therapist, are the treatment of choice. In some cases, transcutaneous electrical nerve stimulation (TENS) with a small battery-operated unit may be used to reduce pain by blocking nerve impulses. If these measures are unsuccessful, an intra-articular injection of steroids into the glenoid humeral joint can result in marked improvement of the frozen shoulder in a large percentage of cases. In those rare people who do not improve from nonoperative measures, manipulation of the shoulder under general anesthesia and an arthroscopic procedure to cut the remaining adhesions can be highly effective in most cases.
Fracture
A fracture involves a partial or total crack through a bone. The break in a bone usually occurs as a result of an impact injury, such as a fall or blow to the shoulder. A fracture usually involves the clavicle or the neck (area below the ball) of the humerus.
- Signs and symptoms. A shoulder fracture that occurs after a major injury is usually accompanied by severe pain. Within a short time, there may be redness and bruising around the area. Sometimes a fracture is obvious because the bones appear out of position.
- Diagnosis. X rays can confirm the diagnosis of a shoulder fracture and the degree of its severity.
- Treatment. When a fracture occurs, the doctor tries to bring the bones into a position that will promote healing and restore arm movement. If someone’s clavicle is fractured, he or she must initially wear a strap and sling around the chest to keep the clavicle in place. After removing the strap and sling, the doctor will prescribe exercises to strengthen the shoulder and restore movement. Surgery is occasionally needed for certain clavicle fractures.
Fracture of the neck of the humerus is usually treated with a sling or shoulder stabilizer. If the bones are out of position, surgery may be necessary to reset them. Exercises are also part of restoring shoulder strength and motion.
Arthritis of the Shoulder
Arthritis is a degenerative disease caused by either wear and tear of the cartilage (osteoarthritis) or an inflammation (rheumatoid arthritis) of one or more joints. Arthritis not only affects joints, but may also affect supporting structures such as muscles, tendons, and ligaments.
- Signs and symptoms. The usual signs of arthritis of the shoulder are pain, particularly over the acromioclavicular joint, and a decrease in shoulder motion.
- Diagnosis. A doctor may suspect the patient has arthritis when there is both pain and swelling in the joint. The diagnosis may be confirmed by a physical examination and x rays. Blood tests may be helpful for diagnosing rheumatoid arthritis, but other tests may be needed as well. Analysis of synovial fluid from the shoulder joint may be helpful in diagnosing some kinds of arthritis. Although arthroscopy permits direct visualization of damage to cartilage, tendons, and ligaments, and may confirm a diagnosis, it is usually done only if a repair procedure is to be performed.
- Treatment. Treatment of shoulder arthritis depends in part on the type of arthritis. Osteoarthritis of the shoulder is usually treated with nonsteroidal anti-inflammatory drugs, such as aspirin and ibuprofen. Rheumatoid arthritis may require physical therapy and additional medications such as corticosteroids.
When nonoperative treatment of arthritis of the shoulder fails to relieve pain or improve function, or when there is severe wear and tear of the joint causing parts to loosen and move out of place, shoulder joint replacement (arthroplasty) may provide better results. In this operation, a surgeon replaces the shoulder joint with an artificial ball for the top of the humerus and a cap (glenoid) for the scapula. Passive shoulder exercises (where someone else moves the arm to rotate the shoulder joint) are started soon after surgery. Patients begin exercising on their own about 3 to 6 weeks after surgery. Eventually, stretching and strengthening exercises become a major part of the rehabilitation program. The success of the operation often depends on the condition of rotator cuff muscles before surgery and the degree to which the patient follows the exercise program.
Treat Shoulder Injuries With RICE
(Rest, Ice, Compression, and Elevation)
If you injure a shoulder, try the following:
Rest. Reduce or stop using the injured area for 48 hours.
Ice. Put an ice pack on the injured area for 20 minutes at a time, 4 to 8 times per day. Use a cold pack, ice bag, or a plastic bag filled with crushed ice that has been wrapped in a towel.
Compression. Compress the area with bandages, such as an elastic wrap, to help stabilize the shoulder. This may help reduce the swelling.
Elevation. Keep the injured area elevated above the level of the heart. Use a pillow to help elevate the injury.
If pain and stiffness persist, see a doctor.
What Do the Knees Do? How Do They Work?
The knee is the joint where the bones of the upper leg meet the bones of the lower leg, allowing hinge-like movement while providing stability and strength to support the weight of the body. Flexibility, strength, and stability are needed for standing and for motions like walking, running, crouching, jumping, and turning.
Several kinds of supporting and moving parts, including bones, cartilage, muscles, ligaments, and tendons, help the knees do their job (see box “Joint Basics”). Each of these structures is subject to disease and injury. When a knee problem affects your ability to do things, it can have a big impact on your life. Knee problems can interfere with many things, from participation in sports to simply getting up from a chair and walking.
- What Causes Knee Problems?
- What Are the Parts of the Knee?
- How Are Knee Problems Diagnosed?
- What Are Some Common Knee Injuries and Problems?
- What Kinds of Doctors Evaluate and Treat Knee Problems?
- How Can People Prevent Knee Problems?
- What Types of Exercise Are Best for People With Knee Problems?
- What Research Is Being Conducted on Knee Problems?
- Where Can People Find More Information About Knee Problems?
- Key Words
Illustration
Information Boxes
Joint Basics
The point at which two or more bones are connected is called a joint. In all joints, the bones are kept from grinding against each other by a lining called cartilage. Bones are joined to bones by strong, elastic bands of tissue called ligaments. Muscles are connected to bones by tough cords of tissue called tendons. Muscles pull on tendons to move joints. Although muscles are not technically part of a joint, they’re important because strong muscles help support and protect joints.
What Causes Knee Problems?
Knee problems can be the result of disease or injury.
Disease
A number of diseases can affect the knee. The most common is arthritis. Although arthritis technically means “joint inflammation,” the term is used loosely to describe many different diseases that can affect the joints. Some of the most common forms of arthritis and their effects on the knees are described a bit later in this publication.
Injury
Knee injuries can occur as the result of a direct blow or sudden movements that strain the knee beyond its normal range of motion. Sometimes knees are injured slowly over time. Problems with the hips or feet, for example, can cause you to walk awkwardly, which throw off the alignment of the knees and leads to damage. Knee problems can also be the result of a lifetime of normal wear and tear. Much like the treads on a tire, the joint simply wears out over time. This publication discusses some of the most common knee injuries, but first describes the structure of the knee joint.
What Are the Parts of the Knee?
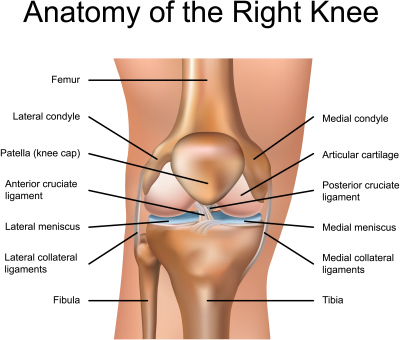
Like any joint, the knee is composed of bones and cartilage, ligaments, tendons, and muscles. Take a closer look at the different parts of the knee in the illustration below.
Bones and Cartilage
The knee joint is the junction of three bones: the femur (thigh bone or upper leg bone), the tibia (shin bone or larger bone of the lower leg), and the patella (kneecap). The patella is 2 to 3 inches wide and 3 to 4 inches long. It sits over the other bones at the front of the knee joint and slides when the knee moves. It protects the knee and gives leverage to muscles.
The ends of the three bones in the knee joint are covered with articular cartilage, a tough, elastic material that helps absorb shock and allows the knee joint to move smoothly. Separating the bones of the knee are pads of connective tissue called menisci (men-NISS-sky). The menisci are two crescent-shaped discs, each called a meniscus (men-NISS-kus), positioned between the tibia and femur on the outer and inner sides of each knee. The two menisci in each knee act as shock absorbers, cushioning the lower part of the leg from the weight of the rest of the body as well as enhancing stability.
Muscles
There are two groups of muscles at the knee. The four quadriceps muscles on the front of the thigh work to straighten the knee from a bent position. The hamstring muscles, which run along the back of the thigh from the hip to just below the knee, help to bend the knee.
Tendons and Ligaments
The quadriceps tendon connects the quadriceps muscle to the patella and provides the power to straighten the knee. The following four ligaments connect the femur and tibia and give the joint strength and stability:
- The medial collateral ligament, which runs along the inside of the knee joint, provides stability to the inner (medial) part of the knee.
- The lateral collateral ligament, which runs along the outside of the knee joint, provides stability to the outer (lateral) part of the knee.
- The anterior cruciate ligament, in the center of the knee, limits rotation and the forward movement of the tibia.
- The posterior cruciate ligament, also in the center of the knee, limits backward movement of the tibia.
The knee capsule is a protective, fiber-like structure that wraps around the knee joint. Inside the capsule, the joint is lined with a thin, soft tissue called synovium.
How Are Knee Problems Diagnosed?
Doctors diagnose knee problems based on the findings of a medical history, physical exam, and diagnostic tests.
Medical History
During the medical history, the doctor asks how long symptoms have been present and what problems you are having using your knee. In addition, the doctor will ask about any injury, condition, or health problem that might be causing the problem.
Physical Examination
The doctor bends, straightens, rotates (turns), or presses on the knee to feel for injury and to determine how well the knee moves and where the pain is located. The doctor may ask you to stand, walk, or squat to help assess the knee’s function.
Diagnostic Tests
Depending on the findings of the medical history and physical exam, the doctor may use one or more tests to determine the nature of a knee problem. Some of the more commonly used tests include:
- X ray (radiography). A procedure in which an x-ray beam is passed through the knee to produce a two-dimensional picture of the bones.
- Computerized axial tomography (CT) scan. A painless procedure in which x rays are passed through the knee at different angles, detected by a scanner, and analyzed by a computer. CT scan images show soft tissues such as ligaments or muscles more clearly than do conventional x rays. The computer can combine individual images to give a three-dimensional view of the knee.
- Bone scan (radionuclide scanning). A technique for creating images of bones on a computer screen or on film. Before the procedure, a harmless radioactive material is injected into your bloodstream. The material collects in the bones, particularly in abnormal areas of the bones, and is detected by a scanner.
- Magnetic resonance imaging (MRI). A procedure that uses a powerful magnet linked to a computer to create pictures of areas inside the knee. During the procedure, your leg is placed in a cylindrical chamber where energy from a powerful magnet (rather than x rays) is passed through the knee. An MRI is particularly useful for detecting soft tissue damage.
- Arthroscopy. A surgical technique in which the doctor manipulates a small, lighted optic tube (arthroscope) that has been inserted into the joint through a small incision in the knee. Images of the inside of the knee joint are projected onto a television screen.
- Joint aspiration. A procedure that uses a syringe to remove fluid buildup in a joint to reduce swelling and relieve pressure. A laboratory analysis of the fluid can determine the presence of a fracture, an infection, or an inflammatory response.
- Biopsy. A procedure in which tissue is removed from the body and studied under a microscope.
What Are Some Common Knee Injuries and Problems?
There are many diseases and types of injuries that can affect the knee. These are some of the most common, along with their diagnoses and treatment.
Arthritis
There are some 100 different forms of arthritis,1 rheumatic diseases, and related conditions. Virtually all of them have the potential to affect the knees in some way; however, the following are the most common.
1 The National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse has separate publications on the different forms of arthritis mentioned in this section. See the end of this publication for contact information.
- Osteoarthritis. Some people with knee problems have a form of arthritis called osteoarthritis. In this disease, the cartilage gradually wears away and changes occur in the adjacent bone. Osteoarthritis may be caused by joint injury or being overweight. It is associated with aging and most typically begins in people age 50 or older. A young person who develops osteoarthritis typically has had an injury to the knee or may have an inherited form of the disease.
- Rheumatoid arthritis. Rheumatoid arthritis, which generally affects people at a younger age than does osteoarthritis, is an autoimmune disease. This means it occurs as a result of the immune system attacking components of the body. In rheumatoid arthritis, the primary site of the immune system’s attack is the synovium, the membrane that lines the joint. This attack causes inflammation of the joint. It can lead to destruction of the cartilage and bone and, in some cases, muscles, tendons, and ligaments as well.
- Other rheumatic diseases. These include:
- Gout. An acute and intensely painful form of arthritis that occurs when crystals of the bodily waste product uric acid are deposited in the joints.
- Systemic lupus erythematosus (lupus). An autoimmune disease characterized by destructive inflammation of the skin, internal organs, and other body systems, as well as the joints.
- Ankylosing spondylitis. An inflammatory form of arthritis that primarily affects the spine, leading to stiffening and in some cases fusing into a stooped position.
- Psoriatic arthritis. A condition in which inflamed joints produce symptoms of arthritis for patients who have or will develop psoriasis.
- Reactive arthritis. A term describing forms of arthritis that are caused by infectious agents, such as bacteria or viruses. Prompt medical attention is essential to treat the infection and minimize damage to joints, particularly if fever is present.
Symptoms
The symptoms are different for the different forms of arthritis. For example, people with rheumatoid arthritis, gout, or other inflammatory conditions may find the knee swollen, red, and even hot to the touch. Any form of arthritis can cause the knee to be painful and stiff.
Diagnosis
The doctor may confirm the diagnosis by conducting a careful history and physical examination. Blood tests may be helpful for diagnosing rheumatoid arthritis, but other tests may also be needed. Analyzing fluid from the knee joint, for example, may be helpful in diagnosing gout. X rays may be taken to determine loss or damage to cartilage or bone.
Treatment
Like the symptoms, treatment varies depending on the form of arthritis affecting the knee. For osteoarthritis, treatment is targeted at relieving symptoms and may include pain-reducing medicines such as aspirin or acetaminophen; nonsteroidal anti-inflammatory drugs (NSAIDs)2 such as ibuprofen; or, in some cases, injections of corticosteroid medications directly into the knee joint3. Other treatments for the pain of knee osteoarthritis include injections of hyaluronic acid substitutes and the nutritional supplements glucosamine and chondroitin sulphate. (For more information about the use of these two supplements, see “What Research Is Being Conducted on Knee Problems.”)
2 Warning: Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other drugs cannot be taken when a patient is being treated with NSAIDs, because NSAIDs alter the way the body uses or eliminates these other drugs. Check with your health care provider or pharmacist before you take NSAIDs. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
3 All medicines can have side effects. Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
People with diseases such as rheumatoid arthritis, ankylosing spondylitis, or psoriatic arthritis often require disease-modifying antirheumatic drugs (DMARDs) or biologic response modifiers (biologics) to control the underlying disease that is the source of their knee problems. These drugs are typically prescribed after less potent treatments, such as NSAIDs or intra-articular injections, are deemed ineffective.
DMARDs are a family of medicines that may be able to slow or stop the immune system from attacking the joints. This in turn prevents pain and swelling. DMARDs typically require regular blood tests to monitor side effects. In addition to relieving signs and symptoms, these drugs may help to retard or even stop joint damage from progressing. However, DMARDs cannot fix joint damage that has already occurred. Some of the most commonly prescribed DMARDs are methotrexate, hydroxychloroquine, sulfasalazine, and leflunomide.
Biologic response modifiers, or biologics, are a new family of genetically engineered drugs that block specific molecular pathways of the immune system that are involved in the inflammatory process. They are often prescribed in combination with DMARDs such as methotrexate. Because biologics work by suppressing the immune system, they could be problematic for patients who are prone to frequent infection. They are typically administered by injection at home or by an intravenous infusion at a clinic.
People with any type of arthritis may benefit from exercises to strengthen the muscles that support the knee and from weight loss, if needed, to relieve excess stress on the joints.
If arthritis causes serious damage to a knee or there is incapacitating pain or loss of use of the knee from arthritis, joint surgery may be considered. Traditionally, this has been done with what is known as a total knee replacement. However, newer surgical procedures are continuously being developed that include resurfacing or replacing only the damaged cartilage surfaces while leaving the rest of the joint intact.
Chondromalacia
Chondromalacia (KON-dro-mah-LAY-she-ah), also called chondromalacia patellae, refers to softening of the articular cartilage of the kneecap. This disorder occurs most often in young adults and can be caused by injury, overuse, misalignment of the patella, or muscle weakness. Instead of gliding smoothly across the lower end of the thigh bone, the kneecap rubs against it, thereby roughening the cartilage underneath the kneecap. The damage may range from a slightly abnormal surface of the cartilage to a surface that has been worn away to the bone. Chondromalacia related to injury occurs when a blow to the kneecap tears off either a small piece of cartilage or a large fragment containing a piece of bone (osteochondral fracture).
Symptoms
The most frequent symptom of chondromalacia is a dull pain around or under the kneecap that worsens when walking down stairs or hills. A person may also feel pain when climbing stairs or when the knee bears weight as it straightens. The disorder is common in runners and is also seen in skiers, cyclists, and soccer players.
Diagnosis
Your description of symptoms and an x ray usually help the doctor make a diagnosis. Although arthroscopy can confirm the diagnosis, it’s not performed unless conservative treatment has failed.
Treatment
Many doctors recommend that people with chondromalacia perform low-impact exercises that strengthen muscles, particularly muscles of the inner part of the quadriceps, without injuring joints. Swimming, riding a stationary bicycle, and using a cross-country ski machine are examples of good exercises for this condition. Electrical stimulation may also be used to strengthen the muscles.
Increasingly, doctors are using osteochondral grafting, in which a plug of bone and healthy cartilage is harvested from one area and transplanted to the injury site. Another relatively new technique is known as autologous chondrocyte implantation (ACI). It involves harvesting healthy cartilage cells, cultivating them in a lab, and implanting them over the lesion.
If these treatments don’t improve the condition, the doctor may perform arthroscopic surgery to smooth the surface of the cartilage and “wash out” the cartilage fragments that cause the joint to catch during bending and straightening. In more severe cases, surgery may be necessary to correct the angle of the kneecap and relieve friction between it and the cartilage, or to reposition parts that are out of alignment.
Meniscal Injuries (Injuries to the Mensici)
The menisci can be easily injured by the force of rotating the knee while bearing weight. A partial or total tear may occur when a person quickly twists or rotates the upper leg while the foot stays still (for example, when dribbling a basketball around an opponent or turning to hit a tennis ball). If the tear is tiny, the meniscus stays connected to the front and back of the knee; if the tear is large, the meniscus may be left hanging by a thread of cartilage. The seriousness of a tear depends on its location and extent.
Symptoms
Generally, when people injure a meniscus, they feel some pain, particularly when the knee is straightened. If the pain is mild, the person may continue moving. Severe pain may occur if a fragment of the meniscus catches between the femur and the tibia. Swelling may occur soon after injury if there is damage to blood vessels. Swelling may also occur several hours later if there is inflammation of the joint lining (synovium). Sometimes, an injury that occurred in the past but was not treated becomes painful months or years later, particularly if the knee is injured a second time. After any injury, the knee may click, lock, feel weak, or give way. Although symptoms of meniscal injury may disappear on their own, they frequently persist or return and require treatment.
Diagnosis
In addition to listening to your description of the onset of pain and swelling, the doctor may perform a physical examination and take x rays of the knee. An MRI may be recommended to confirm the diagnosis. Occasionally, the doctor may use arthroscopy to help diagnose a meniscal tear.
Treatment
If the tear is minor and the pain and other symptoms go away, the doctor may recommend a muscle-strengthening program. The following exercises are designed to build up the quadriceps and hamstring muscles and increase flexibility and strength after injury to the meniscus:
- Warming up the joint by riding a stationary bicycle, then straightening and raising the leg (but not straightening it too much).
- Extending the leg while sitting (a weight may be worn on the ankle for this exercise).
- Raising the leg while lying on the stomach.
- Exercising in a pool (walking as fast as possible in chest-deep water, performing small flutter kicks while holding onto the side of the pool, and raising each leg to 90 degrees in chest-deep water while pressing the back against the side of the pool).
Before beginning any type of exercise program, consult your doctor or physical therapist to learn which exercises are appropriate for you and how to do them correctly, because doing the wrong exercise or exercising improperly can cause problems. A health care professional can also advise you on how to warm up safely and when to avoid exercising a joint affected by arthritis.
If your lifestyle is limited by the symptoms or the problem, the doctor may perform arthroscopic or open surgery to see the extent of injury and to remove or repair the tear. Most young athletes are able to return to active sports after meniscus repair.
Recovery after surgical repair takes several weeks. The best results of treatment for meniscal injury are achieved in people who do not show articular cartilage changes and who have an intact anterior cruciate ligament.
Cruciate Ligament Injuries
Cruciate ligament injuries are sometimes referred to as sprains.4 They don’t necessarily cause pain, but they are disabling. The anterior cruciate ligament is most often stretched or torn (or both) by a sudden twisting motion (for example, when the feet are planted one way and the knees are turned another). The posterior cruciate ligament is most often injured by a direct impact, such as in an automobile accident or football tackle.
4 The National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse has a separate publication on sprains and strains. See the end of this booklet for contact information.
Symptoms
You may hear a popping sound, and the leg may buckle when you try to stand on it.
Diagnosis
The doctor may perform several tests to see whether the parts of the knee stay in proper position when pressure is applied in different directions. A thorough examination is essential. An MRI is accurate in detecting a complete tear, but arthroscopy may be the only reliable means of detecting a partial one.
Treatment
For an incomplete tear, the doctor may recommend an exercise program to strengthen surrounding muscles. He or she may also prescribe a brace to protect the knee during activity. For a completely torn anterior cruciate ligament in an active athlete and motivated person, the doctor is likely to recommend surgery. The surgeon may reconstruct the torn ligament by using a piece (graft) of healthy tissue from you (autograft) or from a cadaver (allograft). Although synthetic ligaments have been tried in experiments, the results have not been as good as with human tissue. One of the most important elements in a successful recovery after cruciate ligament surgery is a 4- to 6-month exercise and rehabilitation program that may involve using special exercise equipment at a rehabilitation or sports center. Successful surgery and rehabilitation will allow the person to return to a normal lifestyle.
Medial and Lateral Collateral Ligament Injuries
The medial collateral ligament is more easily injured than the lateral collateral ligament. The cause of collateral ligament injuries is most often a blow to the outer side of the knee that stretches and tears the ligament on the inner side of the knee. Such blows frequently occur in contact sports such as football or hockey.
Symptoms
When injury to the medial collateral ligament occurs, you may feel a pop and the knee may buckle sideways. Pain and swelling are common.
Diagnosis
A thorough examination is needed to determine the type and extent of the injury. In diagnosing a collateral ligament injury, the doctor exerts pressure on the side of the knee to determine the degree of pain and the looseness of the joint. An MRI is helpful in diagnosing injuries to these ligaments.
Treatment
Most sprains of the collateral ligaments will heal if you follow a prescribed exercise program. In addition to exercise, the doctor may recommend ice packs to reduce pain and swelling, and a small sleeve-type brace to protect and stabilize the knee. A sprain may take 2 to 4 weeks to heal. A severely sprained or torn collateral ligament may be accompanied by a torn anterior cruciate ligament, which usually requires surgical repair.
Tendon Injuries
Knee tendon injuries range from tendinitis (inflammation of a tendon) to a ruptured (torn) tendon. If a person overuses a tendon during certain activities such as dancing, cycling, or running, the tendon stretches and becomes inflamed. Tendinitis of the patellar tendon is sometimes called “jumper’s knee” because in sports that require jumping, such as basketball, the muscle contraction and force of hitting the ground after a jump strain the tendon. After repeated stress, the tendon may become inflamed or tear.
Symptoms
People with tendinitis often have tenderness at the point where the patellar tendon meets the bone. In addition, they may feel pain during running, hurried walking, or jumping. A complete rupture of the quadriceps or patellar tendon is not only painful, but also makes it difficult for a person to bend, extend, or lift the leg against gravity.
Diagnosis
If there is not much swelling, the doctor will be able to feel a defect in the tendon near the tear during a physical examination. An x ray will show that the patella is lower than normal in a quadriceps tendon tear and higher than normal in a patellar tendon tear. The doctor may use an MRI to confirm a partial or total tear.
Treatment
Initially, the treatment for tendinitis involves rest, elevating the knee, applying ice, and taking NSAID medications such as aspirin or ibuprofen to relieve pain and decrease inflammation and swelling. A series of rehabilitation exercises is also useful. If the quadriceps or patellar tendon is completely ruptured, a surgeon will reattach the ends. After surgery, a cast is worn for 3 to 6 weeks and crutches are used. For a partial tear, the doctor might apply a cast without performing surgery.
Rehabilitating a partial or complete tear of a tendon requires an exercise program that is similar to but less vigorous than that prescribed for ligament injuries. The goals of exercise are to restore the ability to bend and straighten the knee and to strengthen the leg to prevent repeat injury. A rehabilitation program may last 6 months, although people can resume many activities before then.
Osgood-Schlatter Disease
Osgood-Schlatter disease is a condition caused by repetitive stress or tension on part of the growth area of the upper tibia (the apophysis). It is characterized by inflammation of the patellar tendon and surrounding soft tissues at the point where the tendon attaches to the tibia. The disease may also be associated with an injury in which the tendon is stretched so much that it tears away from the tibia and takes a fragment of bone with it. The disease most commonly affects active young people, particularly boys between the ages of 10 and 15, who play games or sports that include frequent running and jumping.
Symptoms
People with this disease experience pain just below the knee joint that usually worsens with activity and is relieved by rest. A bony bump that is particularly painful when pressed may appear on the upper edge of the tibia (below the kneecap). Usually, the motion of the knee is not affected. Pain may last a few months and may recur until the child’s growth is completed.
Diagnosis
Osgood-Schlatter disease is most often diagnosed by the symptoms. An x ray may be normal, or show an injury, or, more typically, show that the growth area is in fragments.
Treatment
Osgood-Schlatter disease is temporary and the pain usually goes away without treatment. Applying ice to the knee when pain begins helps relieve inflammation and is sometimes used along with stretching and strengthening exercises. The doctor may advise you to limit participation in vigorous sports. Children who wish to continue moderate or less stressful sports activities may need to wear knee pads for protection and apply ice to the knee after activity. If there is a great deal of pain, sports activities may be limited until the discomfort becomes tolerable.
Iliotibial Band Syndrome
Iliotibial band syndrome is an inflammatory condition caused when a band of tissue rubs over the outer bone (lateral condyle) of the knee. Although iliotibial band syndrome may be caused by direct injury to the knee, it is most often caused by the stress of long-term overuse, such as sometimes occurs in sports training and, particularly, in running.
Symptoms
A person with this syndrome feels an ache or burning sensation at the side of the knee during activity. Pain may be localized at the side of the knee or radiate up the side of the thigh. A person may also feel a snap when the knee is bent and then straightened. Swelling is usually absent, and knee motion is normal.
Diagnosis
The diagnosis of this disorder is typically based on the symptoms, such as pain at the outer bone, and exclusion of other conditions with similar symptoms.
Treatment
Usually, iliotibial band syndrome disappears if the person reduces activity and performs stretching exercises followed by muscle-strengthening exercises. In rare cases when the syndrome doesn’t disappear, surgery may be necessary to split the tendon so it isn’t stretched too tightly over the bone.
Osteochondritis Dissecans
Osteochondritis dissecans results from a loss of the blood supply to an area of bone underneath a joint surface. It usually involves the knee. The affected bone and its covering of cartilage gradually loosen and cause pain. This problem usually arises spontaneously in an active adolescent or young adult. It may be caused by a slight blockage of a small artery or to an unrecognized injury or tiny fracture that damages the overlying cartilage. A person with this condition may eventually develop osteoarthritis.
Lack of a blood supply can cause bone to break down (osteonecrosis).5 The involvement of several joints or the appearance of osteochondritis dissecans in several family members may indicate that the disorder is inherited.
5 The NIAMS Information Clearinghouse has a separate publication on osteonecrosis. See the end of this booklet for contact information.
Symptoms
If normal healing doesn’t occur, cartilage separates from the diseased bone and a fragment breaks loose into the knee joint, causing weakness, sharp pain, and locking of the joint.
Diagnosis
An x ray, MRI, or arthroscopy can determine the condition of the cartilage and can be used to diagnose osteochondritis dissecans.
Treatment
If cartilage fragments have not broken loose, a surgeon may fix them in place with pins or screws that are sunk into the cartilage to stimulate a new blood supply. If fragments are loose, the surgeon may scrape down the cavity to reach fresh bone, add a bone graft, and fix the fragments in position. Fragments that cannot be mended are removed, and the cavity is drilled or scraped to stimulate new cartilage growth. Research is being done to assess the use of cartilage cell and other tissue transplants to treat this disorder.
Plica Syndrome
Plica (PLI-kah) syndrome occurs when plicae (bands of synovial tissue) are irritated by overuse or injury. Synovial plicae are the remains of tissue pouches found in the early stages of fetal development. As the fetus develops, these pouches normally combine to form one large synovial cavity. If this process is incomplete, plicae remain as four folds or bands of synovial tissue within the knee. Injury, chronic overuse, or inflammatory conditions are associated with this syndrome.
Symptoms
Symptoms of plica syndrome include pain and swelling, a clicking sensation, and locking and weakness of the knee.
Diagnosis
Because the symptoms are similar to those of some other knee problems, plica syndrome is often misdiagnosed. Diagnosis usually depends on excluding other conditions that cause similar symptoms.
Treatment
The goal of treatment for plica syndrome is to reduce inflammation of the synovium and thickening of the plicae. The doctor usually prescribes medicine such as ibuprofen to reduce inflammation. People are also advised to reduce activity, apply ice and an elastic bandage to the knee, and do strengthening exercises. A cortisone injection into the plica folds helps about half of those treated. If treatment fails to relieve symptoms within 3 months, the doctor may recommend arthroscopic or open surgery to remove the plicae.
What Kinds of Doctors Evaluate and Treat Knee Problems?
After an examination by your primary care doctor, he or she may refer you to a rheumatologist, an orthopaedic surgeon, or both. A rheumatologist specializes in nonsurgical treatment of arthritis and other rheumatic diseases. An orthopaedic surgeon, or orthopaedist, specializes in nonsurgical and surgical treatment of bones, joints, and soft tissues such as ligaments, tendons, and muscles.
You may also be referred to a physiatrist. Specializing in physical medicine and rehabilitation, physiatrists seek to restore optimal function to people with injuries to the muscles, bones, tissues, and nervous system.
Minor injuries or arthritis may be treated by an internist (a doctor trained to diagnose and treat nonsurgical diseases) or your primary care doctor.
About Total Knee Replacement
Joint replacement is becoming more common, and hips and knees are the most commonly replaced joints. In 2010, 719,000 total knee replacements and 328,000 total hip replacements were performed.
The new joint, called a prosthesis, can be made of plastic, metal, or both. It may be cemented into place or uncemented. An uncemented prosthesis is designed so that bones will grow into it.
First made available in the late 1950s, early total knee replacements did a poor job of mimicking the natural motion of the knee. For that reason, these procedures resulted in high failure and complication rates. Advances in total knee replacement technology in the past 10 to 15 years have enhanced the design and fit of knee implants.
Total knee replacement is often the answer for people when x rays and other tests show joint damage; when moderate-to-severe, persistent pain does not improve adequately with nonsurgical treatment; and when the limited range of motion in their knee joint diminishes their quality of life.
In the past, patients between 60 and 75 years of age were considered to be the best candidates for total knee replacement. Over the past two decades, however, that age range has broadened to include more patients older than 75, who are likely to have other health issues, and patients younger than 60, who are generally more physically active and whose implants will probably be exposed to greater mechanical stress.
About 90 percent of patients appear to experience rapid and substantial reduction in pain, feel better in general, and enjoy improved joint function. Although most total knee replacement surgeries are successful, failure does occur and revision is sometimes necessary. Risk factors include being younger than 55 years old, being male, being obese, and having osteoarthritis, infection, or other illnesses.
How Can People Prevent Knee Problems?
Some knee problems, such as those resulting from an accident, cannot be foreseen or prevented. However, people can prevent many knee problems by following these suggestions:
- Before exercising or participating in sports, warm up by walking or riding a stationary bicycle, then do stretches. Stretching the muscles in the front of the thigh (quadriceps) and back of the thigh (hamstrings) reduces tension on the tendons and relieves pressure on the knee during activity.
- Strengthen the leg muscles by doing specific exercises (for example, by walking up stairs or hills or by riding a stationary bicycle). A supervised workout with weights is another way to strengthen the leg muscles that support the knee.
- Avoid sudden changes in the intensity of exercise. Increase the force or duration of activity gradually.
- Wear shoes that fit properly and are in good condition. This will help maintain balance and leg alignment when walking or running. Flat feet or overpronated feet (feet that roll inward) can cause knee problems. People can often reduce some of these problems by wearing special shoe inserts (orthotics).
- Maintain a healthy weight to reduce stress on the knee. Obesity increases the risk of osteoarthritis of the knee.
What Types of Exercise Are Best for People With Knee Problems?
Ideally, everyone should get three types of exercise regularly:
- Range-of-motion exercises to help maintain normal joint movement and relieve stiffness.
- Strengthening exercises to help keep or increase muscle strength. Keeping muscles strong with exercises, such as walking up stairs, doing leg lifts or dips, or riding a stationary bicycle, helps support and protect the knee.
- Aerobic or endurance exercises to improve function of the heart and circulation and to help control weight. Weight control can be important to people who have arthritis because extra weight puts pressure on many joints. Some studies show that aerobic exercise can reduce inflammation in some joints.
If you already have knee problems, your doctor or physical therapist can help with a plan of exercise that will help the knee(s) without increasing the risk of injury or further damage. As a general rule, you should choose gentle exercises such as swimming, aquatic exercise, or walking rather than jarring exercises such as jogging or high-impact aerobics.
What Is the Difference Between a Sprain and a Strain?
A sprain is a stretch and/or tear of a ligament (a band of fibrous tissue that connects two or more bones at a joint). One or more ligaments can be injured at the same time. The severity of the injury will depend on the extent of injury (whether a tear is partial or complete) and the number of ligaments involved.
A strain is an injury to either a muscle or a tendon (fibrous cords of tissue that connect muscle to bone). Depending on the severity of the injury, a strain may be a simple overstretch of the muscle or tendon, or it can result from a partial or complete tear.
- What Causes a Sprain?
- Where Do Sprains Usually Occur?
- What Are the Signs and Symptoms of a Sprain?
- What Causes a Strain?
- Where Do Strains Usually Occur?
- What Are the Signs and Symptoms of a Strain?
- How Are Sprains and Strains Treated?
- Can Sprains and Strains Be Prevented?
- Where Can People Find More Information About Sprains and Strains?
Information Boxes
Illustrations
What Causes a Sprain?
A sprain can result from a fall, a sudden twist, or a blow to the body that forces a joint out of its normal position and stretches or tears the ligament supporting that joint. Typically, sprains occur when people fall and land on an outstretched arm, slide into a baseball base, land on the side of their foot, or twist a knee with the foot planted firmly on the ground.
Where Do Sprains Usually Occur?
Although sprains can occur in both the upper and lower parts of the body, the most common site is the ankle. It is estimated that more than 628,000 ankle sprains occur in the United States each year.1
1 Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010 Oct 6;92(13):2279-84.
The ankle joint is supported by several lateral (outside) ligaments and medial (inside) ligaments (see fig. 1). Most ankle sprains happen when the foot turns inward as a person runs, turns, falls, or lands on the ankle after a jump. This type of sprain is called an inversion injury. The knee is another common site for a sprain. A blow to the knee or a fall is often the cause; sudden twisting can also result in a sprain (see fig. 2).
Sprains frequently occur at the wrist, typically when people fall and land on an outstretched hand. A sprain to the thumb is common in skiing and other sports. This injury often occurs when a ligament near the base of the thumb (the ulnar collateral ligament of the metacarpophalangeal joint) is torn (see fig. 3).
What Are the Signs and Symptoms of a Sprain?
The usual signs and symptoms include pain, swelling, bruising, instability, and loss of the ability to move and use the joint (called functional ability). However, these signs and symptoms can vary in intensity, depending on the severity of the sprain. Sometimes people feel a pop or tear when the injury happens.
Doctors closely observe an injured site and ask questions to obtain information to diagnose the severity of a sprain. In general, a grade I or mild sprain is caused by overstretching or slight tearing of the ligaments with no joint instability. A person with a mild sprain usually experiences minimal pain, swelling, and little or no loss of functional ability. Bruising is absent or slight, and the person is usually able to put weight on the affected joint.
When to See a Health Care Provider for a Sprain
- You have severe pain and cannot put any weight on the injured joint.
- The injured area looks crooked or has lumps and bumps (other than swelling) that you do not see on the uninjured joint.
- You cannot move the injured joint.
- You cannot walk more than four steps without significant pain.
- Your limb buckles or gives way when you try to use the joint.
- You have numbness in any part of the injured area.
- You see redness or red streaks spreading out from the injury.
- You injure an area that has been injured several times before.
- You have pain, swelling, or redness over a bony part of your foot.
- You are in doubt about the seriousness of the injury or how to care for it.
A grade II or moderate sprain is caused by further, but still incomplete, tearing of the ligament and is characterized by bruising, moderate pain, and swelling. A person with a moderate sprain usually has more difficulty putting weight on the affected joint and experiences some loss of function. An x ray may be needed to help the health care provider determine if a fracture is causing the pain and swelling. Magnetic resonance imaging is occasionally used to help differentiate between a significant partial injury and a complete tear in a ligament, or can be recommended to rule out other injuries.
People who sustain a grade III or severe sprain completely tear or rupture a ligament. Pain, swelling, and bruising are usually severe, and the patient is unable to put weight on the joint. An x ray is usually taken to rule out a broken bone. When diagnosing any sprain, the health care provider will ask the patient to explain how the injury happened. He or she will examine the affected area and check its stability and its ability to move and bear weight.
What Causes a Strain?
A strain is caused by twisting or pulling a muscle or tendon. Strains can be acute or chronic. An acute strain is associated with a recent trauma or injury; it also can occur after improperly lifting heavy objects or overstressing the muscles. Chronic strains are usually the result of overuse: prolonged, repetitive movement of the muscles and tendons.
Where Do Strains Usually Occur?
Two common sites for a strain are the back and the hamstring muscle (located in the back of the thigh). Contact sports such as soccer, football, hockey, boxing, and wrestling put people at risk for strains. Gymnastics, tennis, rowing, golf, and other sports that require extensive gripping can increase the risk of hand and forearm strains. Elbow strains sometimes occur in people who participate in racquet sports, throwing, and contact sports.
What Are the Signs and Symptoms of a Strain?
Typically, people with a strain experience pain, limited motion, muscle spasms, and possibly muscle weakness. They also can have localized swelling, cramping, or inflammation and, with a minor or moderate strain, usually some loss of muscle function. Patients typically have pain in the injured area and general weakness of the muscle when they attempt to move it. Severe strains that partially or completely tear the muscle or tendon are often very painful and disabling.
How Are Sprains and Strains Treated?
Reduce Swelling and Pain
Treatments for sprains and strains are similar and can be thought of as having two stages. The goal during the first stage is to reduce swelling and pain. At this stage, health care providers usually advise patients to follow a formula of rest, ice, compression, and elevation (RICE) for the first 24 to 48 hours after the injury (see the box below). The health care provider also may recommend an over-the-counter or prescription medication to help decrease pain and inflammation.2
2 All medicines can have side effects. Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
For people with a moderate or severe sprain, particularly of the ankle, a hard cast may be applied. This often occurs after the initial swelling has subsided. Severe sprains and strains may require surgery to repair the torn ligaments, muscle, or tendons. Surgery is usually performed by an orthopaedic surgeon.
It is important that moderate and severe sprains and strains be evaluated by a health care provider to allow prompt, appropriate treatment to begin. This box lists some signs that should alert people to consult their health care provider. However, a person who has any concerns about the seriousness of a sprain or strain should always contact a health care provider for advice.
RICE Therapy
- Rest
Reduce regular exercise or activities of daily living as needed. Your health care provider may advise you to put no weight on an injured area for 48 hours. If you cannot put weight on an ankle or knee, crutches may help. If you use a cane or one crutch for an ankle injury, use it on the uninjured side to help you lean away and relieve weight on the injured ankle. - Ice
Apply an ice pack to the injured area for 20 minutes at a time, four to eight times a day. A cold pack, ice bag, or plastic bag filled with crushed ice and wrapped in a towel can be used. To avoid cold injury and frostbite, do not apply the ice for more than 20 minutes. - Compression
Compression of an injured ankle, knee, or wrist may help reduce swelling. Examples of compression bandages are elastic wraps, special boots, air casts, and splints. Ask your health care provider for advice on which one to use and how tight to apply the bandage safely. - Elevation
If possible, keep the injured ankle, knee, elbow, or wrist elevated on a pillow, above the level of the heart, to help decrease swelling.
Begin Rehabilitation
The second stage of treating a sprain or strain is rehabilitation, with the overall goal of improving the condition of the injured area and restoring its function. The health care provider will prescribe an exercise program designed to prevent stiffness, improve range of motion, and restore the joint’s normal flexibility and strength. Some patients may need physical therapy during this stage. When the acute pain and swelling have diminished, the health care provider will instruct the patient to do a series of exercises several times a day. These are very important because they help reduce swelling, prevent stiffness, and restore normal, pain-free range of motion. The health care provider can recommend many different types of exercises, depending on the injury. A patient with an injured knee or foot will work on weight-bearing and balancing exercises. The duration of the program depends on the extent of the injury, but the regimen commonly lasts for several weeks.
Another goal of rehabilitation is to increase strength and regain flexibility. Depending on the patient’s rate of recovery, this process begins about the second week after the injury. The health care provider will instruct the patient to do a series of exercises designed to meet these goals. During this phase of rehabilitation, patients progress to more demanding exercises as pain decreases and function improves.
The final goal is the return to full daily activities, including sports when appropriate. Patients must work closely with their health care health care provider or physical therapist to determine their readiness to return to full activity. Sometimes people are tempted to resume full activity or play sports despite pain or muscle soreness. Returning to full activity before regaining normal range of motion, flexibility, and strength increases the chance of reinjury and may lead to a chronic problem.
The amount of rehabilitation and the time needed for full recovery after a sprain or strain depend on the severity of the injury and individual rates of healing. For example, a mild ankle sprain may require 3 to 6 weeks of rehabilitation; a moderate sprain could require 2 to 3 months. With a severe sprain, it can take 8 to 12 months to return to full activities. Extra care should be taken to avoid reinjury.
Can Sprains and Strains Be Prevented?
People can do many things to help lower their risk of sprains and strains:
- Avoid exercising or playing sports when tired or in pain.
- Maintain a healthy, well-balanced diet to keep muscles strong.
- Maintain a healthy weight.
- Practice safety measures to help prevent falls. For example, keep stairways, walkways, yards, and driveways free of clutter; anchor scatter rugs; and salt or sand icy sidewalks and driveways in the winter.
- Wear shoes that fit properly.
- Replace athletic shoes as soon as the tread wears out or the heel wears down on one side.
- Do stretching exercises daily.
- Be in proper physical condition to play a sport.
- Warm up and stretch before participating in any sport or exercise.
- Wear protective equipment when playing.
- Run on even surfaces.
Sports Injuries
This publication is for athletes at all ages and levels, for people who exercise, as well as for health care professionals, coaches, and others who want to find out more about sports injuries. This publication describes the different types of musculoskeletal sports injuries, how they can be treated and prevented, and recent treatment advances from research. It also highlights risk factors and contains a resource list. If you have further questions after reading this publication, you may wish to discuss them with a health care professional.
Introduction
In recent years, increasing numbers of people of all ages have been heeding their health professionals’ advice to get active for all of the health benefits exercise has to offer. But for some people—particularly those who overdo or who don’t properly train or warm up—these benefits can come at a price: sports injuries.
Fortunately, most sports injuries can be treated effectively, and most people who suffer injuries can return to a satisfying level of physical activity after an injury. Even better, many sports injuries can be prevented if people take the proper precautions.
This publication answers frequently asked questions about sports injuries. It discusses some of the most common injuries and their treatment, and injury prevention. The publication is for anyone who has a sports injury or who is physically active and wants to prevent sports injuries.
It is for casual and more serious athletes as well as the trainers, coaches, and health professionals who deal with sports injuries.
- What Are Sports Injuries?
- What’s the Difference Between Acute and Chronic Injuries?
- What Should I Do if I Suffer an Injury?
- Who Should I See for My Injury?
- How Are Sports Injuries Treated?
- Who Is at Greatest Risk for Sports Injuries?
- What Can Groups at High Risk Do to Prevent Sports Injuries?
- For More Information
Illustrations
Information Boxes
Appendix
- Traumatic Brain and Spinal Cord Injuries
- Bruises
- Sports Injuries in Young Children: Tips for Caregivers
What Are Sports Injuries?
The term “sports injury,” in the broadest sense, refers to the kinds of injuries that most commonly occur during sports or exercise. Some sports injuries result from accidents; others are due to poor training practices, improper equipment, lack of conditioning, or insufficient warm-up and stretching.
Although virtually any part of your body can be injured during sports or exercise, the term is typically reserved for injuries that involve the musculoskeletal system, which includes the muscles, bones, and associated tissues like cartilage. Traumatic brain and spinal cord injuries (relatively rare during sports or exercise) and bruises are considered briefly in the appendix at the end of this publication. Following are some of the most common sports injuries.
Sprains and Strains
A sprain is a stretch or tear of a ligament, the band of connective tissues that joins the end of one bone with another. Sprains are caused by trauma such as a fall or blow to the body that knocks a joint out of position and, in the worst case, ruptures the supporting ligaments. Sprains can range from first degree (minimally stretched ligament) to third degree (a complete tear). Areas of the body most vulnerable to sprains are ankles, knees, and wrists. Signs of a sprain include varying degrees of tenderness or pain; bruising; inflammation; swelling; inability to move a limb or joint; or joint looseness, laxity, or instability.
A strain is a twist, pull, or tear of a muscle or tendon, a cord of tissue connecting muscle to bone. It is an acute, noncontact injury that results from overstretching or overcontraction. Symptoms of a strain include pain, muscle spasm, and loss of strength. Although it’s hard to tell the difference between mild and moderate strains, severe strains not treated professionally can cause damage and loss of function.
Knee Injuries
Because of its complex structure and weight-bearing capacity, the knee is a commonly injured joint.
Lateral View of the Knee

Knee injuries can range from mild to severe. Some of the less severe, yet still painful and functionally limiting, knee problems are runner’s knee (pain or tenderness close to or under the knee cap at the front or side of the knee), iliotibial band syndrome (pain on the outer side of the knee), and tendinitis, also called tendinosis (marked by degeneration within a tendon, usually where it joins the bone).
More severe injuries include bone bruises or damage to the cartilage or ligaments. There are two types of cartilage in the knee. One is the meniscus, a crescent-shaped disc that absorbs shock between the thigh (femur) and lower leg bones (tibia and fibula). The other is a surface-coating (or articular) cartilage. It covers the ends of the bones where they meet, allowing them to glide against one another. The four major ligaments that support the knee are the anterior cruciate ligament (ACL), the posterior cruciate ligament (PCL), the medial collateral ligament (MCL), and the lateral collateral ligament (LCL). (See illustration “Lateral View of the Knee.”)
Knee injuries can result from a blow to or twist of the knee; from improper landing after a jump; or from running too hard, too much, or without proper warm-up.
Compartment Syndrome
In many parts of the body, muscles (along with the nerves and blood vessels that run alongside and through them) are enclosed in a “compartment” formed of a tough membrane called fascia. When muscles become swollen, they can fill the compartment to capacity, causing interference with nerves and blood vessels as well as damage to the muscles themselves. The resulting painful condition is referred to as compartment syndrome.
Compartment syndrome may be caused by a one-time traumatic injury (acute compartment syndrome), such as a fractured bone or a hard blow to the thigh, by repeated hard blows (depending upon the sport), or by ongoing overuse (chronic exertional compartment syndrome), which may occur, for example, in long-distance running.
Shin Splints
Although the term “shin splints” has been widely used to describe any sort of leg pain associated with exercise, the term actually refers to pain along the tibia or shin bone, the large bone in the front of the lower leg. This pain can occur at the front outside part of the lower leg, including the foot and ankle (anterior shin splints) or at the inner edge of the bone where it meets the calf muscles (medial shin splints).
Shin splints are primarily seen in runners, particularly those just starting a running program. Risk factors for shin splints include overuse or incorrect use of the lower leg; improper stretching, warm-up, or exercise technique; overtraining; running or jumping on hard surfaces; and running in shoes that don’t have enough support. These injuries are often associated with flat (overpronated) feet.
Achilles Tendon Injuries
An Achilles tendon injury results from a stretch, tear, or irritation to the tendon connecting the calf muscle to the back of the heel. These injuries can be so sudden and agonizing that they have been known to bring down charging professional football players in shocking fashion.
The most common cause of Achilles tendon tears is a problem called tendinitis, a degenerative condition caused by aging or overuse. When a tendon is weakened, trauma can cause it to rupture. (See illustration “Lateral View of the Ankle.”)
Achilles tendon injuries are common in middle-aged “weekend warriors” who may not exercise regularly or take time to stretch properly before an activity. Among professional athletes, most Achilles injuries seem to occur in quick-acceleration, jumping sports like football and basketball, and almost always end the season’s competition for the athlete.
Lateral View of the Ankle

Common Types of Sports Injuries
- Muscle sprains and strains
- Tears of the ligaments that hold joints together
- Tears of the tendons that support joints and allow them to move
- Dislocated joints
- Fractured bones, including vertebrae.
Fractures
A fracture is a break in the bone that can occur from either a quick, one-time injury to the bone (acute fracture) or from repeated stress to the bone over time (stress fracture).
Acute fractures: Acute fractures can be simple (a clean break with little damage to the surrounding tissue) or compound (a break in which the bone pierces the skin with little damage to the surrounding tissue). Most acute fractures are emergencies. One that breaks the skin is especially dangerous because there is a high risk of infection.
Stress fractures: Stress fractures occur largely in the feet and legs and are common in sports that require repetitive impact, primarily running/jumping sports such as gymnastics or track and field. Running creates forces two to three times a person’s body weight on the lower limbs.
The most common symptom of a stress fracture is pain at the site that worsens with weight-bearing activity. Tenderness and swelling often accompany the pain.
Dislocations
When the two bones that come together to form a joint become separated, the joint is described as being dislocated. Contact sports such as football and basketball, as well as high-impact sports and sports that can result in excessive stretching or falling, cause the majority of dislocations. A dislocated joint is an emergency situation that requires medical treatment.
The Shoulder Joint

The joints most likely to be dislocated are some of the hand joints. Aside from these joints, the joint most frequently dislocated is the shoulder. (See illustration “The Shoulder Joint.”) Dislocations of the knees, hips, and elbows are uncommon.
What’s the Difference Between Acute and Chronic Injuries?
Regardless of the specific structure affected, sports injuries can generally be classified in one of two ways: acute or chronic.
Acute Injuries
Acute injuries, such as a sprained ankle, strained back, or fractured hand, occur suddenly during activity. Signs of an acute injury include the following:
- sudden, severe pain
- swelling
- inability to place weight on a lower limb
- extreme tenderness in an upper limb
- inability to move a joint through its full range of motion
- extreme limb weakness
- visible dislocation or break of a bone.
Chronic Injuries
Chronic injuries usually result from overusing one area of the body while playing a sport or exercising over a long period. The following are signs of a chronic injury:
- pain when performing an activity
- a dull ache when at rest
- swelling.
What Should I Do if I Suffer an Injury?
Whether an injury is acute or chronic, there is never a good reason to try to “work through” the pain of an injury. When you have pain from a particular movement or activity, STOP! Continuing the activity only causes further harm.
Some injuries require prompt medical attention (see the section “Who Should I See for My Injury?”), while others can be self-treated. Here’s what you need to know about both types:
When to Seek Medical Treatment
You should call a health professional if:
- The injury causes severe pain, swelling, or numbness.
- You can’t tolerate any weight on the area.
- The pain or dull ache of an old injury is accompanied by increased swelling or joint abnormality or instability.
To learn about treating sports injuries, see the section “How Are Sports Injuries Treated?”
When and How to Treat at Home
If you don’t have any of the above symptoms, it’s probably safe to treat the injury at home—at least at first. If pain or other symptoms worsen, it’s best to check with your health care provider. Use the RICE method to relieve pain and inflammation and speed healing. Follow these four steps immediately after injury and continue for at least 48 hours.
- Rest. Reduce regular exercise or activities of daily living as needed. If you cannot put weight on an ankle or knee, crutches may help. If you use a cane or one crutch for an ankle injury, use it on the uninjured side to help you lean away and relieve weight on the injured ankle.
- Ice. Apply an ice pack to the injured area for 20 minutes at a time, four to eight times a day. A cold pack, ice bag, or plastic bag filled with crushed ice and wrapped in a towel can be used. To avoid cold injury and frostbite, do not apply the ice for more than 20 minutes. (Note: Do not use heat immediately after an injury. This tends to increase internal bleeding or swelling. Heat can be used later on to relieve muscle tension and promote relaxation.)
- Compression. Compression of the injured area may help reduce swelling. Compression can be achieved with elastic wraps, special boots, air casts, and splints. Ask your health care provider for advice on which one to use.
- Elevation. If possible, keep the injured ankle, knee, elbow, or wrist elevated on a pillow, above the level of the heart, to help decrease swelling.
The Body’s Healing Process
From the moment a bone breaks or a ligament tears, your body goes to work to repair the damage. Here’s what happens at each stage of the healing process:
At the moment of injury: Chemicals are released from damaged cells, triggering a process called inflammation. Blood vessels at the injury site become dilated; blood flow increases to carry nutrients to the site of tissue damage.
Within hours of injury: White blood cells (leukocytes) travel down the bloodstream to the injury site where they begin to tear down and remove damaged tissue, allowing other specialized cells to start developing scar tissue.
Within days of injury: Scar tissue is formed on the skin or inside the body. The amount of scarring may be proportional to the amount of swelling, inflammation, or bleeding within. In the next few weeks, the damaged area will regain a great deal of strength as scar tissue continues to form.
Within a month of injury: Scar tissue may start to shrink, bringing damaged, torn, or separated tissues back together. However, it may be several months or more before the injury is completely healed.
Who Should I See for My Injury?
Although severe injuries will need to be seen immediately in an emergency room, particularly if they occur on the weekend or after office hours, most sports injuries can be evaluated and, in many cases, treated by your primary health care provider.
Depending on your preference and the severity of your injury or the likelihood that your injury may cause ongoing, long-term problems, you may want to see, or have your primary health care professional refer you to, one of the following:
- An orthopaedic surgeon is a doctor specializing in the diagnosis and treatment of the musculoskeletal system, which includes bones, joints, ligaments, tendons, muscles, and nerves.
- A physical therapist/physiotherapist is a health care professional who can develop a rehabilitation program. Your primary care physician may refer you to a physical therapist after you begin to recover from your injury to help strengthen muscles and joints and prevent further injury.
How Are Sports Injuries Treated?
Although using the RICE technique described previously can be helpful for any sports injury, RICE is often just a starting point. Here are some other treatments your doctor or other health care provider may administer, recommend, or prescribe to help your injury heal.1
1All medicines can have side effects. Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
The moment you are injured, chemicals are released from damaged tissue cells. This triggers the first stage of healing: inflammation (see the box “The Body’s Healing Process”). Inflammation causes tissues to become swollen, tender, and painful. Although inflammation is needed for healing, it can actually slow the healing process if left unchecked.
To reduce inflammation and pain, doctors and other health care providers often recommend taking an over-the-counter (OTC) nonsteroidal anti-inflammatory drug (NSAID) such as aspirin, ibuprofen (Advil,2 Motrin IB, Nuprin), ketoprofen (Actron, Orudis KT), or naproxen sodium (Aleve). For more severe pain and inflammation, doctors may prescribe one of several dozen NSAIDs available in prescription strength.3
2Brand names included in this booklet are provided as examples only, and their inclusion does not mean that these products are endorsed by the National Institutes of Health or any other Government agency. Also, if a particular brand name is not mentioned, this does not mean or imply that the product is unsatisfactory.
3 Warning: Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other drugs cannot be taken when a patient is being treated with NSAIDs, because NSAIDs alter the way the body uses or eliminates these other drugs. Check with your health care provider or pharmacist before you take NSAIDs. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
Though not an NSAID, another commonly used OTC medication, acetaminophen (Tylenol), may relieve pain. It has no effect on inflammation, however.
Immobilization
Immobilization is a common treatment for sports injuries that may be done immediately by a trainer or paramedic. Immobilization involves reducing movement in the area to prevent further damage. By enabling the blood supply to flow more directly to the injury (or the site of surgery to repair damage from an injury), immobilization reduces pain, swelling, and muscle spasm and helps the healing process begin. Following are some devices used for immobilization:
- Slings, to immobilize the upper body, including the arms and shoulders.
- Splints and casts, to support and protect injured bones and soft tissue. Casts can be made from plaster or fiberglass. Splints can be custom made or ready made. Standard splints come in a variety of shapes and sizes and have Velcro straps that make them easy to put on and take off or adjust. Splints generally offer less support and protection than a cast, and therefore may not always be a treatment option.
- Leg immobilizers, to keep the knee from bending after injury or surgery. Made from foam rubber covered with fabric, leg immobilizers enclose the entire leg, fastening with Velcro straps.
Surgery
In some cases, surgery is needed to repair torn connective tissues or to realign bones with compound fractures. The vast majority of sports injuries, however, do not require surgery.
Rehabilitation (Exercise)
A key part of rehabilitation from sports injuries is a graduated exercise program designed to return the injured body part to a normal level of function.
With most injuries, early mobilization—getting the part moving as soon as possible—will speed healing. Generally, early mobilization starts with gentle range-of-motion exercises and then moves on to stretching and strengthening exercise when you can without increasing pain. For example, if you have a sprained ankle, you may be able to work on range of motion for the first day or two after the sprain by gently tracing letters with your big toe. Once your range of motion is fairly good, you can start doing gentle stretching and strengthening exercises. When you are ready, weights may be added to your exercise routine to further strengthen the injured area. The key is to avoid movement that causes pain.
As damaged tissue heals, scar tissue forms, which shrinks and brings torn or separated tissues back together. As a result, the injury site becomes tight or stiff, and damaged tissues are at risk of reinjury. That’s why stretching and strengthening exercises are so important. You should continue to stretch the muscles daily and as the first part of your warm-up before exercising.
When planning your rehabilitation program with a health care professional, remember that progression is the key principle. Start with just a few exercises, do them often, and then gradually increase how much you do. A complete rehabilitation program should include exercises for flexibility, endurance, and strength; instruction in balance and proper body mechanics related to the sport; and a planned return to full participation.
Throughout the rehabilitation process, avoid painful activities and concentrate on those exercises that will improve function in the injured part. Don’t resume your sport until you are sure you can stretch the injured tissues without any pain, swelling, or restricted movement, and monitor any other symptoms. When you do return to your sport, start slowly and gradually build up to full participation. For more advice on how to prevent injuries as you return to active exercise, see the box “Tips for Preventing Injury.”
Rest
Although it is important to get moving as soon as possible, you must also take time to rest following an injury. All injuries need time to heal; proper rest will help the process. Your health care professional can guide you regarding the proper balance between rest and rehabilitation.
Other Therapies
Other therapies used in rehabilitating sports injuries include:
- Electrostimulation: Mild electrical current provides pain relief by preventing nerve cells from sending pain impulses to the brain. Electrostimulation may also be used to decrease swelling, and to make muscles in immobilized limbs contract, thus preventing muscle atrophy and maintaining or increasing muscle strength.
- Cold/cryotherapy: Ice packs reduce inflammation by constricting blood vessels and limiting blood flow to the injured tissues. Cryotherapy eases pain by numbing the injured area. It is generally used for only the first 48 hours after injury.
- Heat/thermotherapy: Heat, in the form of hot compresses, heat lamps, or heating pads, causes the blood vessels to dilate and increase blood flow to the injury site. Increased blood flow aids the healing process by removing cell debris from damaged tissues and carrying healing nutrients to the injury site. Heat also helps to reduce pain. It should not be applied within the first 48 hours after an injury.
- Ultrasound: High-frequency sound waves produce deep heat that is applied directly to an injured area. Ultrasound stimulates blood flow to promote healing.
- Massage: Manual pressing, rubbing, and manipulation soothe tense muscles and increase blood flow to the injury site.
Most of these therapies are administered or supervised by a licensed health care professional.
Who Is at Greatest Risk for Sports Injuries?
If a professional athlete dislocates a joint or tears a ligament, it makes the news. But anyone who plays sports can be injured. Three groups—children and adolescents, middle-aged athletes, and women—are particularly vulnerable.
Children and Adolescents
Although playing sports can improve children’s fitness, self-esteem, coordination, and self-discipline, it can also put them at risk for sports injuries: some minor, some serious, and still others that may result in lifelong medical problems.
Young athletes are not small adults. Their bones, muscles, tendons, and ligaments are still growing and that makes them more prone to injury. Growth plates—the areas of developing cartilage where bone growth occurs in growing children—are weaker than the nearby ligaments and tendons. As a result, what is often a bruise or sprain in an adult can be a potentially serious growth-plate injury in a child. Also, a trauma that would tear a muscle or ligament in an adult would be far more likely to break a child’s bone.
Because young athletes of the same age can differ greatly in size and physical maturity, some may try to perform at levels beyond their ability to keep up with their peers.
Contact sports have inherent dangers that put young athletes at special risk for severe injuries. Even with rigorous training and proper safety equipment, youngsters are still at risk for severe injuries to the neck, spinal cord, and growth plates. Evaluating potential sports injuries on the field in very young children can involve its own special issues for concerned parents and coaches. Some helpful hints are presented in the appendix.
Adult Athletes
More adults than ever are participating in sports. Many factors contribute to sports injuries as the body grows older. The main one is that adults may not be as agile and resilient as they were when they were younger. It is also possible that some injuries occur when a person tries to move from inactive to a more active lifestyle too quickly.
Women
More women of all ages are participating in sports than ever before. In women’s sports, the action is now faster and more aggressive and powerful than in the past. As a result, women are sustaining many more injuries, and the injuries tend to be sport-specific.
Female athletes have higher injury rates than men in many sports, particularly basketball, soccer, alpine skiing, volleyball, and gymnastics. Female college basketball players are about six times more likely to suffer a tear of the knee’s anterior cruciate ligament (ACL) than men are, according to a study of 11,780 high school and college players. Information on injuries collected since 1982 by the National Collegiate Athletic Association shows that female basketball and soccer players have a much higher incidence of ACL injuries than their male counterparts.
Previous assumptions that methods of training, risks of participation, and effects of exercise are the same for men and women are being challenged. Scientists are working to understand the gender differences in sports injuries.
Although poor conditioning has not been related to an increased incidence of ACL injuries specifically, it has been associated with an increase in injuries in general. For most American women, the basic level of conditioning is much lower than that of men. Studies at the U.S. Naval Academy revealed that overuse injuries were more frequent in women; however, as women became used to the rigors of training, the injury rates for men and women became similar.
Aside from conditioning level, other possible factors in women’s sports injuries include structural difference of the knee and thigh muscles, fluctuating estrogen levels caused by menstruation, the fit of athletic shoes, and the way players jump, land, and twist. Also, “the female triad,” a combination of disordered eating, curtailed menstruation (amenorrhea), and loss of bone mass (osteoporosis), is increasingly more common in female athletes in some sports.
What Can Groups at High Risk Do to Prevent Sports Injuries?
Anyone who exercises is potentially at risk for a sports injury and should follow the injury prevention tips in the box “Tips for Preventing Injury.” But additional measures can be taken by groups at higher risk of injury.
Children
Preventing injuries in children is a team effort, requiring the support of parents, coaches, and the kids themselves. Here’s what each should do to reduce injury risk.
What parents and coaches can do:
- Try to group youngsters according to skill level and size, not by chronological age, particularly during contact sports. If this is not practical, modify the sport to accommodate the needs of children with varying skill levels.
- Match the child to the sport, and don’t push the child too hard into an activity that she or he may not like or be physically capable of doing.
- Try to find sports programs where certified athletic trainers are present. These people, in addition to health care professionals, are trained to prevent, recognize, and give immediate care to sports injuries.
- See that all children get a preseason physical exam.
- Don’t let (or insist that) a child play when injured. No child (or adult) should ever be allowed to work through the pain.
- Get the child medical attention if needed. A child who develops any symptom that persists or that affects athletic performance should be examined by a health care professional. Other clues that a child needs to see a health professional include inability to play following a sudden injury, visible abnormality of the arms and legs, and severe pain that prevents the use of an arm or leg.
- Provide a safe environment for sports. A poor playing field, unsafe gym sets, unsecured soccer goals, etc., can cause serious injury to children.
What children can do:
- Be in proper condition to play the sport. Get a preseason physical exam.
- Follow the rules of the game.
- Wear appropriate protective gear.
- Know how to use athletic equipment.
- Avoid playing when very tired or in pain.
- Make warm-ups and cool-downs part of your routine. Warm-up exercises, such as stretching or light jogging, can help minimize the chances of muscle strain or other soft tissue injury. They also make the body’s tissues warmer and more flexible. Cool-down exercises loosen the muscles that have tightened during exercise.
Tips for Preventing Injury
Whether you’ve never had a sports injury and you’re trying to keep it that way or you’ve had an injury and don’t want another, the following tips can help.
- Avoid bending knees past 90 degrees when doing half knee bends.
- Avoid twisting knees by keeping feet as flat as possible during stretches.
- When jumping, land with your knees bent.
- Do warm-up exercises not just before vigorous activities like running, but also before less vigorous ones such as golf.
- Don’t overdo.
- Do warm-up stretches before activity. Stretch the Achilles tendon, hamstring, and quadriceps areas and hold the positions. Don’t bounce.
- Cool down following vigorous sports. For example, after a race, walk or walk/jog for 5 minutes so your pulse comes down gradually.
- Wear properly fitting shoes that provide shock absorption and stability.
- Use the softest exercise surface available, and avoid running on hard surfaces like asphalt and concrete. Run on flat surfaces. Running uphill may increase the stress on the Achilles tendon and the leg itself.
Adult Athletes
To prevent injuries, adult athletes should take the following precautions:
- Don’t be a “weekend warrior,” packing a week’s worth of activity into a day or two. Try to maintain a moderate level of activity throughout the week.
- Learn to do your sport right. Using proper form can reduce your risk of “overuse” injuries such as tendinitis and stress fractures.
- Remember safety gear. Depending on the sport, this may mean knee or wrist pads or a helmet.
- Accept your body’s limits. You may not be able to perform at the same level you did 10 or 20 years ago. Modify activities as necessary.
- Increase your exercise level gradually.
- Strive for a total body workout of cardiovascular, strength training, and flexibility exercises. Cross-training reduces injury while promoting total fitness.
Women
Increased emphasis on muscle strength and conditioning should be a priority for all women. Women should also be encouraged to maintain a normal body weight and avoid excessive exercise that affects the menstrual cycle. In addition, women should follow precautions listed above for other groups.
What Is Osteoarthritis?
Affects Many Older People
Osteoarthritis is the most common form of arthritis among older people, and it is one of the most frequent causes of physical disability among older adults.
The disease affects both men and women. Before age 45, osteoarthritis is more common in men than in women. After age 45, osteoarthritis is more common in women. It is estimated that 33.6% (12.4 million) of individuals age 65 and older are affected by the disease.
Osteoarthritis occurs when cartilage, the tissue that cushions the ends of the bones within the joints, breaks down and wears away. In some cases, all of the cartilage may wear away, leaving bones that rub up against each other.
Joint Stiffness and Pain
Symptoms range from stiffness and mild pain that comes and goes to severe joint pain. Osteoarthritis affects hands, low back, neck, and weight-bearing joints such as knees, hips, and feet. osteoarthritis affects just joints, not internal organs.
Hands
Osteoarthritis of the hands seems to run in families. If your mother or grandmother has or had osteoarthritis in their hands, you’re at greater-than-average risk of having it too. Women are more likely than men to have osteoarthritis in the hands. For most women, it develops after menopause.
When osteoarthritis involves the hands, small, bony knobs may appear on the end joints (those closest to the nails) of the fingers. They are called Heberden’s (HEBerr-denz) nodes. Similar knobs, called Bouchard’s (boo-SHARDZ) nodes, can appear on the middle joints of the fingers. Fingers can become enlarged and gnarled, and they may ache or be stiff and numb. The base of the thumb joint also is commonly affected by osteoarthritis.
Knees
The knees are among the joints most commonly affected by osteoarthritis. Symptoms of knee osteoarthritis include stiffness, swelling, and pain, which make it hard to walk, climb, and get in and out of chairs and bathtubs. Osteoarthritis in the knees can lead to disability.
Hips
The hips are also common sites of osteoarthritis. As with knee osteoarthritis, symptoms of hip osteoarthritis include pain and stiffness of the joint itself. But sometimes pain is felt in the groin, inner thigh, buttocks, or even the knees. Osteoarthritis of the hip may limit moving and bending, making daily activities such as dressing and putting on shoes a challenge.
Spine
Osteoarthritis of the spine may show up as stiffness and pain in the neck or lower back. In some cases, arthritis-related changes in the spine can cause pressure on the nerves where they exit the spinal column, resulting in weakness, tingling, or numbness of the arms and legs. In severe cases, this can even affect bladder and bowel function.
Osteoarthritis
This publication is for people who have osteoarthritis, their families, and others interested in learning more about the disorder. The publication describes osteoarthritis and its symptoms and contains information about diagnosis and treatment, as well as research efforts supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and other components of the U.S. Department of Health and Human Services’ National Institutes of Health (NIH). It also discusses pain relief, exercise, and quality of life for people with osteoarthritis. At the end is a list of key words to help you understand the terms used in this publication. If you have further questions after reading this, you may wish to discuss them with your doctor.
What Is Osteoarthritis?
Osteoarthritis (AH-stee-oh-ar-THREYE-tis) is the most common type of arthritis and is seen especially among older people. Sometimes it is called degenerative joint disease. Osteoarthritis mostly affects cartilage (KAR-til-uj), the hard but slippery tissue that covers the ends of bones where they meet to form a joint. Healthy cartilage allows bones to glide over one another. It also absorbs energy from the shock of physical movement. In osteoarthritis, the surface layer of cartilage breaks and wears away. This allows bones under the cartilage to rub together, causing pain, swelling, and loss of motion of the joint. Over time, the joint may lose its normal shape. Also, small deposits of bone—called osteophytes or bone spurs—may grow on the edges of the joint. Bits of bone or cartilage can break off and float inside the joint space. This causes more pain and damage.
- Who Has Osteoarthritis?
- How Does Osteoarthritis Affect People?
- Osteoarthritis Basics: The Joint and Its Parts
- How Do You Know if You Have Osteoarthritis?
- How Do Doctors Diagnose Osteoarthritis?
- How Is Osteoarthritis Treated?
- Who Provides Care for People With Osteoarthritis?
- What You Can Do: the Importance of Self-Care and a Good-Health Attitude
- Research Highlights
- Hope for the Future
- For More Information
- Key Words
Illustrations
- What Areas Does Osteoarthritis Affect?
- A Healthy Joint
- A Joint With Severe Osteoarthritis
- Exercises for Osteoarthritis
Information Boxes
- Cartilage: The Key to Healthy Joints
- The Warning Signs of Osteoarthritis
- Four Goals of Osteoarthritis Treatment
- Treatment Approaches to Osteoarthritis
- On the Move: Fighting Osteoarthritis with Exercise
- Questions To Ask Your Doctor or Pharmacist About Medicines
- Self-Management Programs Do Help
- Enjoy a Good Health Attitude
People with osteoarthritis usually have joint pain and stiffness. Unlike some other forms of arthritis, such as rheumatoid arthritis, osteoarthritis affects only joint function. It does not affect skin tissue, the lungs, the eyes, or the blood vessels.
In rheumatoid arthritis, another common form of arthritis, the immune system attacks the tissues of the joints, leading to pain, inflammation, and eventually joint damage and malformation. It typically begins at a younger age than osteoarthritis, causes swelling and redness in joints, and may make people feel sick, tired, and feverish. Also, the joint involvement of rheumatoid arthritis is symmetrical; that is, if one joint is affected, the same joint on the opposite side of the body is usually similarly affected. Osteoarthritis, on the other hand, can occur in a single joint or can affect a joint on one side of the body much more severely.
Who Has Osteoarthritis?
Osteoarthritis is by far the most common type of arthritis, and the percentage of people who have it grows higher with age. An estimated 27 million Americans age 25 and older have osteoarthritis.1
1Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Gabriel S, Hirsch R, Hochberg MC, Hunder GG, Jordan JM, Katz JN, Kremers HM, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2008 Jan;58(1):26-35.
Although osteoarthritis becomes more common with age, younger people can develop it, usually as the result of a joint injury, a joint malformation, or a genetic defect in joint cartilage. Both men and women have the disease. Before age 45, more men than women have osteoarthritis; after age 45, it is more common in women. It is also more likely to occur in people who are overweight and in those with jobs that stress particular joints.
How Does Osteoarthritis Affect People?
People with osteoarthritis usually experience joint pain and stiffness. The most commonly affected joints are those at the ends of the fingers (closest to the nail), thumbs, neck, lower back, knees, and hips.
Osteoarthritis affects different people differently. It may progress quickly, but for most people, joint damage develops gradually over years. In some people, osteoarthritis is relatively mild and interferes little with day-to-day life; in others, it causes significant pain and disability.
Although osteoarthritis is a disease of the joints, its effects are not just physical. In many people with osteoarthritis, lifestyle and finances also decline.
What Areas Does Osteoarthritis Affect?

Osteoarthritis most often occurs in the hands (at the ends of the fingers and thumbs), spine (neck and lower back), knees, and hips
Lifestyle effects include:
- depression
- anxiety
- feelings of helplessness
- limitations on daily activities
- job limitations
- difficulty participating in everyday personal and family joys and responsibilities.
Fortunately, most people with osteoarthritis live active, productive lives despite these limitations. They do so by using treatment strategies such as rest and exercise, pain relief medications, education, and support programs; learning self-care; and working to maintain a positive attitude.
Osteoarthritis Basics: The Joint and Its Parts
A joint is the point where two or more bones are connected. With a few exceptions (in the skull and pelvis, for example), joints are designed to allow movement between the bones and to absorb shock from movements like walking or repetitive motions. These movable joints are made up of the following parts:
Cartilage: A hard but slippery coating on the end of each bone. Cartilage, which breaks down and wears away in osteoarthritis, is described in more detail in “Cartilage: The Key to Healthy Joints.”
Joint capsule: A tough membrane sac that encloses all the bones and other joint parts.
Synovium (sin-O-vee-um): A thin membrane inside the joint capsule that secretes synovial fluid.
Synovial fluid: A fluid that lubricates the joint and keeps the cartilage smooth and healthy.
Ligaments, tendons, and muscles: Tissues that surround the bones and joints, and allow the joints to bend and move. Ligaments are tough, cord-like tissues that connect one bone to another.
Tendons: Tough, fibrous cords that connect muscles to bones. Muscles are bundles of specialized cells that, when stimulated by nerves, either relax or contract to produce movement.
A Healthy Joint (Representation)

In a healthy joint, the ends of bones are encased in smooth cartilage. Together, they are protected by a joint capsule lined with a synovial membrane that produces synovial fluid. The capsule and fluid protect the cartilage, muscles, and connective tissues.
A Joint With Severe Osteoarthritis (Representation)

With osteoarthritis, the cartilage becomes worn away. Spurs grow out from the edge of the bone, and synovial fluid increases. Altogether, the joint feels stiff and sore.
Cartilage: The Key to Healthy Joints
Cartilage is 65 to 80 percent water. The remaining three components—collagen, proteoglycans, and chondrocytes—are described below.
- Collagen (KAHL-uh-jen): A family of fibrous proteins, collagens are the building blocks of skin, tendon, bone, and other connective tissues.
- Proteoglycans (PRO-tee-uh-GLY-kanz): Made up of proteins and sugars, strands of proteoglycans interweave with collagens and form a mesh-like tissue. This allows cartilage to flex and absorb physical shock.
- Chondrocytes (KAHN-druh-sytz): Found throughout the cartilage, chondrocytes are cells that produce cartilage and help it stay healthy as it grows. Sometimes, however, they release substances called enzymes that destroy collagen and other proteins. Researchers are trying to learn more about chondrocytes.
How Do You Know if You Have Osteoarthritis?
Usually, osteoarthritis comes on slowly. Early in the disease, your joints may ache after physical work or exercise. Later on, joint pain may become more persistent. You may also experience joint stiffness, particularly when you first wake up in the morning or have been in one position for a long time.
Although osteoarthritis can occur in any joint, most often it affects the hands, knees, hips, and spine (either at the neck or lower back). Different characteristics of the disease can depend on the specific joint(s) affected. For general warning signs of osteoarthritis, see the information box “The Warning Signs of Osteoarthritis.” For information on the joints most often affected by osteoarthritis, see the following descriptions:
Hands: Osteoarthritis of the hands seems to have some hereditary characteristics; that is, it runs in families. If your mother or grandmother has or had osteoarthritis in their hands, you’re at greater-than-average risk of having it too. Women are more likely than men to have osteoarthritis in the hands. For most women, it develops after menopause.
When osteoarthritis involves the hands, small, bony knobs may appear on the end joints (those closest to the nails) of the fingers. They are called Heberden’s (HEBerr-denz) nodes. Similar knobs, called Bouchard’s (boo-SHARDZ) nodes, can appear on the middle joints of the fingers. Fingers can become enlarged and gnarled, and they may ache or be stiff and numb. The base of the thumb joint also is commonly affected by osteoarthritis.
Knees: The knees are among the joints most commonly affected by osteoarthritis. Symptoms of knee osteoarthritis include stiffness, swelling, and pain, which make it hard to walk, climb, and get in and out of chairs and bathtubs. Osteoarthritis in the knees can lead to disability.
Hips: The hips are also common sites of osteoarthritis. As with knee osteoarthritis, symptoms of hip osteoarthritis include pain and stiffness of the joint itself. But sometimes pain is felt in the groin, inner thigh, buttocks, or even the knees. Osteoarthritis of the hip may limit moving and bending, making daily activities such as dressing and putting on shoes a challenge.
Spine: Osteoarthritis of the spine may show up as stiffness and pain in the neck or lower back. In some cases, arthritis-related changes in the spine can cause pressure on the nerves where they exit the spinal column, resulting in weakness, tingling, or numbness of the arms and legs. In severe cases, this can even affect bladder and bowel function.
The Warning Signs of Osteoarthritis
- Stiffness in a joint after getting out of bed or sitting for a long time
- Swelling in one or more joints
- Crunching feeling or the sound of bone rubbing on bone
About a third of people whose x rays show evidence of osteoarthritis report pain or other symptoms. For those who experience steady or intermittent pain, it is typically aggravated by activity and relieved by rest.
If you feel hot or your skin turns red, or if your joint pain is accompanied by other symptoms such as a rash or fevers, you probably do not have osteoarthritis. Check with your doctor about other causes, such as rheumatoid arthritis.
How Do Doctors Diagnose Osteoarthritis?
No single test can diagnose osteoarthritis; however, sometimes doctors use tests to help confirm a diagnosis or rule out other conditions that could be causing your symptoms. Most doctors use a combination of the following methods:
Clinical History
The doctor begins by asking you to describe the symptoms, and when and how the condition started, as well as how the symptoms have changed over time. The doctor will also ask about any other medical problems you and close family members have and about any medications you are taking. Accurate answers to these questions can help the doctor make a diagnosis and understand the impact the disease has on your life.
Physical Examination
The doctor will check your reflexes and general health, including muscle strength. The doctor will also examine bothersome joints and observe your ability to walk, bend, and carry out activities of daily living.
X Rays
X rays can help doctors determine the form of arthritis a person has and how much joint damage has been done. X rays of the affected joint can show such things as cartilage loss, bone damage, and bone spurs. But there often is a big difference between the severity of osteoarthritis as shown by the x ray and the degree of pain and disability you feel. Also, x rays may not show early osteoarthritis damage until much cartilage loss has taken place.
Magnetic Resonance Imaging
Also known as MRI, magnetic resonance imaging provides high-resolution computerized images of internal body tissues. This procedure uses a strong magnet that passes a force through the body to create these images. Doctors often use MRI tests if there is pain; if x-ray findings are minimal; and if the findings suggest damage to other joint tissues such as a ligament or the pad of connective tissue in the knee known as the meniscus.
Other Tests
The doctor may order blood tests to rule out other causes of symptoms. He or she may also order a joint aspiration, which involves drawing fluid from the joint through a needle and examining the fluid under a microscope. Joint fluid samples could reveal bacteria, indicating joint pain is caused by an infection or uric acid crystals, indicating gout.
Osteoarthritis is so common, especially in older people, that symptoms seemingly caused by the disease actually may be caused by other medical conditions. The doctor will try to find out what is causing the symptoms by ruling out other disorders and identifying conditions that may make the symptoms worse. The severity of symptoms in osteoarthritis can be influenced greatly by your attitude, anxiety, depression, and daily activity level.
How Is Osteoarthritis Treated?
Most successful treatment programs involve a combination of approaches tailored to the patient’s needs, lifestyle, and health. Most programs include ways to manage pain and improve function. These can involve exercise, weight control, rest and relief from stress on joints, pain relief techniques, medications, surgery, and complementary and alternative therapies. These approaches are described below.
Four Goals of Osteoarthritis Treatment
- to control pain
- to improve joint function
- to maintain normal body weight
- to achieve a healthy lifestyle.
Treatment Approaches to Osteoarthritis
- exercise
- weight control
- rest and relief from stress on joints
- nondrug pain relief techniques and alternative therapies
- medications to control pain
- surgery.
Exercise
Research shows that exercise is one of the best treatments for osteoarthritis. Exercise can improve mood and outlook, decrease pain, increase flexibility, strengthen the heart and improve blood flow, maintain weight, and promote general physical fitness. Exercise is also inexpensive and, if done correctly, has few negative side effects. The amount and form of exercise prescribed will depend on which joints are involved, how stable the joints are, and whether a joint replacement has already been done. Walking, swimming, and water aerobics are a few popular types of exercise for people with osteoarthritis. Your doctor and/or physical therapist can recommend specific types of exercise depending on your particular situation. (See section “What You Can Do: The Importance of Self-Care and a Good Health Attitude”).
On the Move: Fighting Osteoarthritis With Exercise
You can use exercises to keep strong and limber, improve cardiovascular fitness, extend your joints’ range of motion, and reduce your weight. The following types of exercise are part of a well-rounded arthritis treatment plan.
- Strengthening exercises: These exercises strengthen muscles that support joints affected by arthritis. They can be performed with weights or with exercise bands, inexpensive devices that add resistance.
- Aerobic activities: These are exercises, such as brisk walking or low-impact aerobics, that get your heart pumping and can keep your lungs and circulatory system in shape.
- Range-of-motion activities: These keep your joints limber.
- Balance and agility exercises: These help you maintain daily living skills.
Ask your doctor or physical therapist what exercises are best for you. Ask for guidelines on exercising.
Weight Control
If you are overweight or obese, you should try to lose weight. Weight loss can reduce stress on weight-bearing joints, limit further injury, increase mobility, and reduce the risk of associated health problems. A dietitian can help you develop healthy eating habits. A healthy diet and regular exercise help reduce weight.
Rest and Relief from Stress on Joints
Treatment plans include regularly scheduled rest. You must learn to recognize the body’s signals, and know when to stop or slow down. This will prevent the pain caused by overexertion. Although pain can make it difficult to sleep, getting proper sleep is important for managing arthritis pain. If you have trouble sleeping, you may find that relaxation techniques, stress reduction, and biofeedback can help, as can timing medications to provide maximum pain relief through the night. If joint pain interferes with your ability to sleep or rest, consult your doctor.
Some people find relief from special footwear and insoles that can reduce pain and improve walking or from using canes to take pressure off painful joints. They may use splints or braces to provide extra support for joints and/ or keep them in proper position during sleep or activity. Splints should be used only for limited periods of time because joints and muscles need to be exercised to prevent stiffness and weakness. If you need a splint, an occupational therapist or a doctor can help you get a properly fitted one.
Nondrug Pain Relief and Alternative Therapies
People with osteoarthritis may find many nondrug ways to relieve pain. Below are some examples:
Heat and cold: Heat or cold (or a combination of the two) can be useful for joint pain. Heat can be applied in a number of different ways—with warm towels, hot packs, or a warm bath or shower—to increase blood flow and ease pain and stiffness. In some cases, cold packs (bags of ice or frozen vegetables wrapped in a towel), which reduce inflammation, can relieve pain or numb the sore area. (Check with a doctor or physical therapist to find out if heat or cold is the best treatment.)
Transcutaneous electrical nerve stimulation (TENS):TENS is a technique that uses a small electronic device to direct mild electric pulses to nerve endings that lie beneath the skin in the painful area. TENS may relieve some arthritis pain. It seems to work by blocking pain messages to the brain and by modifying pain perception.
Massage: In this pain-relief approach, a massage therapist will lightly stroke and/or knead the painful muscles. This may increase blood flow and bring warmth to a stressed area. However, arthritis-stressed joints are sensitive, so the therapist must be familiar with the problems of the disease.
Acupuncture: When conventional medical treatment doesn’t provide sufficient pain relief, people are more likely to try complementary and alternative therapies to treat osteoarthritis. Some people have found pain relief usingacupuncture, a practice in which fine needles are inserted by a licensed acupuncture therapist at specific points on the skin. Scientists think the needles stimulate the release of natural, pain-relieving chemicals produced by the nervous system. A large study supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Center for Complementary and Alternative Medicine (NCCAM) revealed that acupuncture relieves pain and improves function in knee osteoarthritis, and it serves as an effective complement to standard care.2
2Berman BM, Lao L, Langenberg P, Lee WL, Gilpin AM, Hochberg MC. Effectiveness of acupuncture as adjunctive therapy in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2004 Dec 21;141(12):901-10.
Nutritional supplements, such as glucosamine and chondroitin sulfate have been reported to improve symptoms in some people with osteoarthritis, as have certain vitamins. Additional studies have been carried out to further evaluate these claims (see “Research Highlights”). It is unknown whether they might change the course of disease.
Medications to Control Pain
Doctors prescribe medicines to eliminate or reduce pain and to improve functioning. Doctors consider a number of factors when choosing medicines for their patients with osteoarthritis. These include the intensity of pain, potential side effects of the medication, your medical history (other health problems you have or are at risk for), and other medications you are taking.
Because some medications can interact with one another and certain health conditions put you at increased risk of drug side effects, it’s important to discuss your medication and health history with your doctor before you start taking any new medication, and to see your doctor regularly while you are taking medication. By working together, you and your doctor can find the medication that best relieves your pain with the least risk of side effects.
The following types of medicines are commonly used in treating osteoarthritis:3
3All medicines can have side effects. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
Over-the-counter pain relievers: Oral pain medications, such as acetaminophen, are often a first-line approach to relieve pain in people with osteoarthritis.
NSAIDs (nonsteroidal anti-inflammatory drugs): A large class of medications useful against both pain and inflammation, (NSAIDs)4 are staples in arthritis treatment. Aspirin, ibuprofen, naproxen, and naproxen sodium are examples of NSAIDs. They are often the first type of medication used. All NSAIDs work similarly: by blocking substances called prostaglandins that contribute to inflammation and pain. However, each NSAID is a different chemical, and each has a slightly different effect on the body.
4 Warning: Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other drugs cannot be taken when a patient is being treated with NSAIDs, because NSAIDs alter the way the body uses or eliminates these other drugs. Check with your health care provider or pharmacist before you take NSAIDs. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
Some NSAIDs are available over the counter, while more than a dozen others, including a subclass called COX-2 inhibitors, are available only with a prescription.
All NSAIDs can have significant side effects, and for unknown reasons, some people seem to respond better to one NSAID than another. Any person taking NSAIDs regularly should be monitored by a doctor.
Reducing the Risks of NSAID Use
Certain health problems and lifestyle habits can increase the risk of side effects from NSAIDs. These include a history of peptic ulcers or digestive tract bleeding, use of oral corticosteroids or anticoagulants (blood thinners), smoking, and alcohol use.
There are measures you can take to help reduce the risk of side effects associated with NSAIDs. These include taking medications with food and avoiding stomach irritants such as alcohol, tobacco, and caffeine. In some cases, it may help to take another medication along with an NSAID to coat the stomach or block stomach acids. Although these measures may help, they are not always completely effective.
Narcotic or central acting agents: Tramadol is a prescription pain reliever and synthetic opioid that is sometimes prescribed when over-the-counter medications don’t provide sufficient relief. It works through the central nervous system to achieve its effects. Tramadol carries risks that don’t exist with acetaminophen and NSAIDs, including the potential for addiction.
Mild narcotic painkillers containing analgesics such as codeine or hydrocodone are often effective against osteoarthritis pain. But because of concerns about the potential for physical and psychological dependence on these drugs, doctors generally reserve them for short-term use.
Corticosteroids: Corticosteroids are powerful anti- inflammatory hormones made naturally in the body or man-made for use as medicine. They may be injected into the affected joints to temporarily relieve pain. This is a short-term measure, generally not recommended for more than two to four treatments per year. Oral corticosteroids are not routinely used to treat osteoarthritis. They are occasionally used for inflammatory flares.
Hyaluronic acid substitutes: Sometimes called viscosupplements, hyaluronic acid substitutes are designed to replace a normal component of the joint involved in joint lubrication and nutrition. Depending on the particular product your doctor prescribes, it will be given in a series of three to five injections. These products are approved only for osteoarthritis of the knee.
Other medications: Doctors may prescribe several other medicines for osteoarthritis. They include topical pain-relieving creams, rubs, and sprays, which are applied directly to the skin over painful joints. They contain ingredients that work in one of three different ways: (1) by stimulating the nerve endings to distract the brain’s attention from the joint pain, (2) by depleting the amount of a neurotransmitter called substance P that sends pain messages to the brain, or (3) by blocking chemicals called prostaglandins that cause pain and inflammation.
Because most medicines used to treat osteoarthritis have side effects, it’s important to learn as much as possible about the medications you take, even the ones available without a prescription. Certain health problems and lifestyle habits can increase the risk of side effects from NSAIDs. These include a history of peptic ulcers or digestive tract bleeding, use of oral corticosteroids or anticoagulants (blood thinners), smoking, and alcohol use.
There are measures you can take to help reduce the risk of side effects associated with NSAIDs. These include taking medications with food and avoiding stomach irritants such as alcohol, tobacco, and caffeine. In some cases, it may help to take another medication along with an NSAID to coat the stomach or block stomach acids. Although these measures may help, they are not always completely effective.
Questions to Ask Your Doctor or Pharmacist About Medicines
- How often should I take this medicine?
- Should I take this medicine with food or between meals?
- What side effects might occur?
- Should I take this medicine with the other prescription medicines I take?
- Is this medication safe considering other medical conditions I have?
Surgery
For many people, surgery helps relieve the pain and disability of osteoarthritis. Surgery may be performed to achieve one or more of the following:
- Removal of loose pieces of bone and cartilage from the joint if they are causing symptoms of buckling or locking (arthroscopic debridement).
- Repositioning of bones (osteotomy).
- Resurfacing (smoothing out) bones (joint resurfacing).
Surgeons may replace affected joints with artificial joints called prostheses. These joints can be made from metal alloys, high-density plastic, and ceramic material. Some prostheses are joined to bone surfaces with special cements. Others have porous surfaces and rely on the growth of bone into that surface (a process called biologic fixation) to hold them in place. Artificial joints can last 10 to 15 years or longer. Surgeons choose the design and components of prostheses according to their patient’s weight, sex, age, activity level, and other medical conditions.
Joint replacement advances in recent years have included the ability, in some cases, to replace only the damaged part of the knee joint, leaving undamaged parts of the joint intact, and the ability to perform hip replacement through much smaller incisions than previously possible.
The decision to use surgery depends on several factors, including the patient’s age, occupation, level of disability, pain intensity, and the degree to which arthritis interferes with his or her lifestyle. After surgery and rehabilitation, the patient usually feels less pain and swelling and can move more easily.
Who Provides Care for People With Osteoarthritis?
Treating arthritis often requires a multidisciplinary or team approach. Many types of health professionals care for people with arthritis. You may choose a few or more of the following professionals to be part of your health care team:
Primary care physicians: Doctors who treat patients before they are referred to other specialists in the health care system. Often a primary care physician will be the main doctor to treat your arthritis. Primary care physicians also handle other medical problems and coordinate the care you receive from other physicians and health care providers.
Rheumatologists: Doctors who specialize in treating arthritis and related conditions that affect joints, muscles, and bones.
Orthopaedists: Surgeons who specialize in the treatment of, and surgery for, bone and joint diseases.
Physical therapists: Health professionals who work with patients to improve joint function.
Occupational therapists: Health professionals who teach ways to protect joints, minimize pain, perform activities of daily living, and conserve energy.
Dietitians: Health professionals who teach ways to use a good diet to improve health and maintain a healthy weight.
Nurse educators: Nurses who specialize in helping patients understand their overall condition and implement their treatment plans.
Physiatrists (rehabilitation specialists): Medical doctors who help patients make the most of their physical potential.
Licensed acupuncture therapists: Health professionals who reduce pain and improve physical functioning by inserting fine needles into the skin at specific points on the body.
Psychologists: Health professionals who seek to help patients cope with difficulties in the home and workplace resulting from their medical conditions.
Social workers: Professionals who assist patients with social challenges caused by disability, unemployment, financial hardships, home health care, and other needs resulting from their medical conditions.
Chiropractors: Health professionals who focus treatment on the relationship between the body’s structure—mainly the spine—and its functioning.
Massage therapists: Health professionals who press, rub, and otherwise manipulate the muscles and other soft tissues of the body. They most often use their hands and fingers, but may use their forearms, elbows, or feet.
What You Can Do: The Importance of Self-Care and a Good Health Attitude
Although health care professionals can prescribe or recommend treatments to help you manage your arthritis, the real key to living well with the disease is you. Research shows that people with osteoarthritis who take part in their own care report less pain and make fewer doctor visits. They also enjoy a better quality of life.
Living well and enjoying good health despite arthritis requires an everyday lifelong commitment. The following six habits are worth committing to:
1. Get educated: To live well with osteoarthritis, it pays to learn as much as you can about the disease. Three kinds of programs help people understand osteoarthritis, learn self-care, and improve their good-health attitude. They are:
- patient education programs
- arthritis self-management programs
- arthritis support groups.
These programs teach people about osteoarthritis, its treatments, exercise and relaxation, patient and health care provider communication, and problem solving. Research has shown that people who participate in these programs are more likely to have positive outcomes.
Self-Management Programs Do Help
People with osteoarthritis find that self-management programs help them:
- understand the disease
- reduce pain while remaining active
- cope physically, emotionally, and mentally
- have greater control over the disease
- build confidence in their ability to live an active, independent life.
2. Stay active: Regular physical activity plays a key role in self-care and wellness. Four types of exercise are important in osteoarthritis management. The first type, strengthening exercises help keep or increase muscle strength. Strong muscles help support and protect joints affected by arthritis. The second type, aerobic conditioning exercises improve cardiovascular fitness, help control weight, and improve overall function. The third type, range-of-motion exercises, help reduce stiffness and maintain or increase proper joint movement and flexibility. The fourth type, balance and agility exercises, can help you maintain daily living skills.
You should start each exercise session with an adequate warm-up and begin exercising slowly. Resting frequently ensures a good workout and reduces the risk of injury.
Before beginning any type of exercise program, consult your doctor or physical therapist to learn which exercises are appropriate for you and how to do them correctly, because doing the wrong exercise or exercising improperly can cause problems. A health care professional can also advise you on how to warm up safely and when to avoid exercising a joint affected by arthritis.
Exercises for Osteoarthritis

People with osteoarthritis should do different kinds of exercise for different benefits to the body. Consult your health professional before starting. The National Institute on Aging Web site (www.nia.nih.gov) has booklets on exercise and physical activity that may also be helpful.
3. Eat well: Though no specific diet will necessarily make your arthritis better, eating right and controlling your weight can help by minimizing stress on the weight-bearing joints such as the knees and the joints of the feet. It can also minimize your risk of developing other health problems.
4. Get plenty of sleep: Getting a good night’s sleep on a regular basis can minimize pain and help you cope better with the effects of your disease. If arthritis pain makes it difficult to sleep at night, speak with your doctor and/or physical therapist about the best mattress or comfortable sleeping positions or the possibility of timing medications to provide more pain relief at night. You may also improve your sleep by getting enough exercise early in the day; avoiding caffeine or alcoholic beverages at night; keeping your bedroom dark, quiet, and cool; and taking a warm bath to relax and soothe sore muscles at bedtime.
5. Have fun: Although having osteoarthritis certainly isn’t fun, it doesn’t mean you have to stop having fun. If arthritis makes it difficult to participate in favorite activities, ask an occupational therapist about new ways to do them. Activities such as sports, hobbies, and volunteer work can distract your mind from your own pain and make you a happier, more well-rounded person.
Enjoy a “Good Health Attitude”
- Focus on your abilities instead of disabilities.
- Focus on your strengths instead of weaknesses.
- Break down activities into small tasks that you can manage.
- Incorporate fitness and nutrition into daily routines.
- Develop methods to minimize and manage stress.
- Balance rest with activity.
- Develop a support system of family, friends, and health professionals.
6. Keep a positive attitude: Perhaps the best thing you can do for your health is to keep a positive attitude. People must decide to make the most of things when faced with the challenges of osteoarthritis. This attitude—a good-health mindset—doesn’t just happen. It takes work, every day. And with the right attitude, you will achieve it.
Research Highlights
The leading role in osteoarthritis research is played by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), part of the National Institutes of Health (NIH). The NIAMS funds many researchers across the United States to study osteoarthritis.
One of the major areas of focus of osteoarthritis research in recent years has been the potential role of inflammation in the disease. One NIAMS-supported study found that a pathway called the complement system, which is a major component of the innate immune system, is critical to the development of osteoarthritis. Through analyses of joint tissue and joint fluid from individuals with osteoarthritis, researchers found that expression and activation of complement is abnormally high in people with osteoarthritis. The innate immune system is designed to protect the body from harmful invaders such as viruses and bacteria. When cartilage is injured, the researchers found, the complement system is activated, leading to inflammation directed against the body’s own tissues.
The researchers confirmed the role in mice, which are an animal model for osteoarthritis. They found the mice developed a disease characteristic of human osteoarthritis following injury to the stabilizing ligament of the knee joint. When the scientists genetically engineered those mice to lack part of the complement system’s, however, they did not develop osteoarthritis. The same results were seen when the mice were treated with an agent to inhibit part of the complement system, confirming its role in the development of the disease.
If these findings about the complement’s role hold true in people, blocking a part of the complement system may be an effective treatment for early osteoarthritis. Other key areas of research supported by the NIAMS and other institutes within NIH include the following:
Biomarkers
In 2004, the NIAMS and other institutes and offices of the NIH began recruiting participants for the Osteoarthritis Initiative (OAI). The OAI is a public-private partnership that brings together new resources and a commitment to help identify biomarkers of disease for osteoarthritis. The partnership is designed to stimulate the development of tools and identify targets to combat the disease. Biomarkers are biological clues to increased disease susceptibility, early stages of disease, the course of the disease, and the response of people with osteoarthritis to the various therapies. Researchers are collecting images (x rays and MRIs), biological specimens (blood, urine, and DNA), and clinical data from 4,800 people at high risk for having osteoarthritis, as well as those at high risk for progression to severe osteoarthritis during the course of the study.
This groundbreaking study is expected to advance our understanding of how modifiable and non-modifiable risk factors are linked to development and worsening of knee osteoarthritis. Such findings may, in turn, lead to improved strategies for prevention of disease and identification of novel treatment targets, which could result in prevention of later-life disability in individuals with knee osteoarthritis.
Two separate NIAMS-supported studies revealed that mechanical stress can affect the release of osteoarthritis biomarkers. The first study, on the role of mechanical stress on biomarker release from normal cartilage, showed that mechanical stress in the ranges experienced from normal to intense physical activity increased the turnover of cartilage and the release of biomarkers from the tissue and varied with the amount of applied stress. This suggests that mechanical stress regulates turnover of molecules in the cartilage extracellular matrix. The second study, which examined release of cartilage-and bone-derived biomarkers in college athletes undergoing high-intensity training (rowers, cross-country runners, and swimmers) and in nonathlete controls, suggests that rowers undergo the highest bone turnover and runners the highest cartilage turnover. These results suggest that biomarkers can vary between individuals involved in different types of physical activities, and that the interpretation of biomarker analyses from osteoarthritis patients will need to take into account the type and extent of physical activity of the patients.
Diagnostic Tools
A recently discovered method to detect and monitor cartilage changes could eventually enable doctors to diagnose osteoarthritis long before traditional x rays would show damage. It could also allow clinicians the opportunity to monitor the impact of therapeutic interventions very early in the disease process. The new noninvasive method uses an adaptation of established MRI techniques to separately visualize proteoglycans (molecular building blocks of cartilage) from water molecules in cartilage. Although further research and refinements are needed, the researchers are hopeful this approach could one day play an important role in the management of people with osteoarthritis.
Other NIAMS-supported researchers are combining a technique called microcomputed tomography (microCT), which yields high-resolution, three-dimensional x-ray images, with an x-ray-absorbing contrast agent to image the distribution of proteoglycans in the laboratory. By detecting proteoglycan content and distribution, the technique reveals information about both the thickness and composition of cartilage, both of which are important factors for monitoring the progression and treatment of osteoarthritis. So far, the technique’s use has been limited to cartilage samples from animals. The researchers don’t know yet if the technique would be successful in people. The hope is that their research will lead to ways to monitor cartilage changes with good resolution and little or no invasion of the tissue, and that eventually the technique will allow pharmaceutical researchers to obtain more detailed information about the effects of new drugs and other treatment strategies for osteoarthritis.
Pharmacologic Treatments
One drug that has been studied is the osteoporosis medication risedronate. In a British study of several hundred people with mild-to-moderate osteoarthritis of the knee, those treated with risedronate, a member of a class of drugs called bisphosphonates, showed a clear trend toward reduced symptoms and improved joint structure.
Researchers supported by the NIAMS have shown that teriparatide, a form of human parathyroid hormone that triggers new bone formation and is approved to treat osteoporosis, can restore cartilage in a mouse model of injury-induced osteoarthritis of the knee. More studies are needed for both drugs.
Complementary and Alternative Therapies
In recent years, the nutritional supplement pair glucosamine and chondroitin has shown some potential for reducing the pain of osteoarthritis, though no conclusive proof has emerged to date. Both of these nutrients are found in shark cartilage, the shells of shellfish, and pig ears and noses, and are components of normal cartilage.
The Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT), which was cosponsored by the National Center for Complementary and Alternative Medicine (NCCAM) and the NIAMS, assessed the effectiveness and safety of these supplements when taken together or separately. The trial found that the combination of glucosamine and chondroitin sulfate did not provide significant relief from osteoarthritis pain among all participants. However, a subgroup of study participants with moderate-to-severe pain showed significant relief with the combined supplements. The 4-year trial was conducted at 16 sites across the United States.
There are other complementary and alternative therapies under investigation. For example, a recent study found that a 60-minute “dose” of Swedish massage therapy delivered once a week for pain caused by osteoarthritis of the knee was both optimal and practical, establishing a standard for use in future research. This trial, funded by NCCAM, builds on an earlier pilot study of massage for knee osteoarthritis pain, which had promising results but provided no data to determine whether the dose was optimal. (The researchers defined an optimal, practical dose as producing the greatest ratio of desired effect compared to costs in time, labor, and convenience.)
The researchers noted that there is promising potential for the use of massage therapy for osteoarthritis of the knee and that future, larger trials should use this dose as a standard. Furthermore, they suggest that more definitive research is needed on massage for osteoarthritis of the knee, in terms of efficacy, how it may work in the body, and its cost effectiveness for patients.
Other research has shown that a deficiency of vitamin K—a fat-soluble vitamin found in leafy green vegetables such as broccoli, kale, spinach, and lettuces—is associated with the development of knee osteoarthritis. One recent study showed that although supplements of vitamin K appear to have no effect on osteoarthritis in most people, for people who are deficient in vitamin K, supplements could have a significant effect. In the study, participants who had insufficient levels of vitamin K at baseline but achieved sufficient concentrations at followup had almost 50 percent less joint space narrowing (a sign of cartilage damage) in their hands.
Healing Joint Injuries and Cartilage Damage
When the anterior cruciate ligament (ACL)—one of the main ligaments of the knee, which connects the shin bone to the thigh—is torn, it doesn’t heal the way other tissues do. Unless the tear is repaired, the knee can become unstable, resulting in damage to the joint surfaces and the eventual development of knee osteoarthritis. Traditionally, repair has involved replacing the ligament with ligament or tendon graft, but NIAMS-funded research shows that filling the tear with a collagen- and platelet-rich gel material may enable it to heal, making a graft unnecessary. Physicians believe that preserving the patient’s own ACL (if it becomes possible) would likely better protect the mechanics of the knee.
Other NIAMS-supported scientists are researching a way to patch damaged cartilage that will allow new cartilage to grow in and repair the damage. Using a unique weaving machine of their own design, the researchers have created a three-dimensional fabric scaffold patch. In laboratory tests, the scaffold had the same mechanical properties as native cartilage. In the future, surgeons will likely be able to impregnate custom-designed scaffold with cartilage-forming stem cells (taken from a person’s own fat tissue, for example) and biochemicals that stimulate their growth, and then implant them into a patient in a single procedure.
Genetics Studies
Osteoarthritis in all its various forms appears to have a strong but complex genetic connection. Gene mutations may be a factor in predisposing individuals to develop osteoarthritis. For example, scientists have identified a mutation (a gene defect) affecting collagen, an important part of cartilage, in patients with an inherited kind of osteoarthritis that starts at an early age. The mutation weakens collagen protein, which may break or tear more easily under stress.
The Johnston County Osteoarthritis Project, a University of North Carolina study focusing on a group of 5,000 adults, age 45 or older, identified six genes—ABCG2, GDF5, IL1RN, IL6, and VDR—that appear to increase susceptibility to knee osteoarthritis.
Patient Education and Self-Management
When patients understand and feel that they have some control over their chronic disease, the course of their disease is often improved. One NIAMS-supported study found that improvement can be made in the self-management of osteoarthritis when spouses provide help. The intervention that was tested used spouse-assisted coping skills training and exercise training to improve physical fitness, pain coping, and self-efficacy in patients with osteoarthritis of the knee. The results from the study suggest that a combination of both spouse-assisted pain coping skills training and exercise training leads to more improvements than could be achieved with either intervention alone.
Other research shows that patient education and social support is a low-cost, effective way to decrease pain and reduce the amount of medicine patients use. One NIAMS-funded project involves developing and testing an interactive website by which health professionals and patients could communicate concerning appointments and treatment instructions, thus giving patients a greater role in and control of their care.
Exercise and Weight Reduction
Exercise plays a key part in a comprehensive treatment plan. Researchers are studying exercise in greater detail and finding out just how to use it in treating or preventing osteoarthritis. For example, several scientists have studied knee osteoarthritis and exercise. Their results included the following:
- Walking can result in better functioning, and the more you walk, the farther you will be able to walk.
- People with knee osteoarthritis who are active in an exercise program feel less pain. They also function better.
Research has shown that losing extra weight can help people who already have osteoarthritis. Moreover, overweight or obese people who do not have osteoarthritis may reduce their risk of developing the disease by losing weight.
Rheumatoid Arthritis
This publication is for people who have rheumatoid arthritis, as well as for their family members, friends, and others who want to find out more about this disease. The publication describes how rheumatoid arthritis develops, how it is diagnosed, and how it is treated, including what people can do to help manage their disease. It also highlights current research efforts supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and other components of the U.S. Department of Health and Human Services’ National Institutes of Health (NIH). If you have further questions after reading this publication, you may wish to discuss them with your doctor.
What Is Rheumatoid Arthritis?
- Who Has Rheumatoid Arthritis?
- What Happens in Rheumatoid Arthritis?
- How Does Rheumatoid Arthritis Affect People’s Lives?
- What Causes Rheumatoid Arthritis?
- How Is Rheumatoid Arthritis Diagnosed?
- How Is Rheumatoid Arthritis Treated?
- Who Treats Rheumatoid Arthritis?
- What You Can Do: The Importance of Self-Care
- What Research Is Being Conducted on Rheumatoid Arthritis?
- Hope for the Future
- Key Words
Illustration
Information Boxes
Rheumatoid arthritis has several features that make it different from other kinds of arthritis. (See box “Features of Rheumatoid Arthritis.”) For example, rheumatoid arthritis generally occurs in a symmetrical pattern, meaning that if one knee or hand is involved, the other one also is. The disease often affects the wrist joints and the finger joints closest to the hand. It can also affect other parts of the body besides the joints. (See “What Happens in Rheumatoid Arthritis?”) In addition, people with rheumatoid arthritis may have fatigue, occasional fevers, and a loss of energy.
Features of Rheumatoid Arthritis
- Tender, warm, swollen joints
- Symmetrical pattern of affected joints
- Joint inflammation often affecting the wrist and finger joints closest to the hand
- Joint inflammation sometimes affecting other joints, including the neck, shoulders, elbows, hips, knees, ankles, and feet
- Fatigue, occasional fevers, a loss of energy
- Pain and stiffness lasting for more than 30 minutes in the morning or after a long rest
- Symptoms that last for many years
- Variability of symptoms among people with the disease
Rheumatoid arthritis (RA) is an inflammatory disease that causes pain, swelling, stiffness, and loss of function in the joints. It occurs when the immune system, which normally defends the body from invading organisms, turns its attack against the membrane lining the joints.
The course of rheumatoid arthritis can range from mild to severe. In most cases it is chronic, meaning it lasts a long time—often a lifetime. For many people, periods of relatively mild disease activity are punctuated by flares, or times of heightened disease activity. In others, symptoms are constant.
Who Has Rheumatoid Arthritis?
Scientists estimate that about 1.5 million people, or about 0.6 percent of the U.S. adult population, have rheumatoid arthritis.1 Interestingly, some recent studies have suggested that although the number of new cases of rheumatoid arthritis for older people is increasing, the overall number of new cases may actually be going down.
1According to the National Arthritis Data Workgroup, the actual number of new cases of rheumatoid arthritis is lower than previous estimates because of changes in the classification for the condition, as cited in Helmick CG, Felson DT, Lawrence RC, Gabriel S, Hirsch R, Kwoh CK, Liang MH, Kremers HM, Mayes MD, Merkel PA, Pillemer SR, Reveille JD, Stone JH, for the National Arthritis Data Workgroup. Estimates of the Prevalence of Arthritis and Other Rheumatic Conditions in the United States. Part I. Arthritis Rheum 2008;58(1):15-25.
Rheumatoid arthritis occurs in all races and ethnic groups. Although the disease often begins in middle age and occurs with increased frequency in older people, older teenagers and young adults may also be diagnosed with the disease. (Children and younger teenagers may be diagnosed with juvenile idiopathic arthritis, a condition related to rheumatoid arthritis.) Like some other forms of arthritis, rheumatoid arthritis occurs much more frequently in women than in men. About two to three times as many women as men have the disease.
What Happens in Rheumatoid Arthritis?
Rheumatoid arthritis is primarily a disease of the joints. A joint is the point where two or more bones come together. With a few exceptions (in the skull and pelvis, for example), joints are designed to allow movement between the bones and to absorb shock from movements like walking or repetitive motions. The ends of the bones are covered by a tough, elastic tissue called cartilage. The joint is surrounded by a capsule that protects and supports it (see illustration). The joint capsule is lined with a type of tissue called synovium, which produces synovial fluid, a clear substance that lubricates and nourishes the cartilage and bones inside the joint capsule.
Like many other rheumatic diseases, rheumatoid arthritis is an autoimmune disease (auto means self), so-called because a person’s immune system, which normally helps protect the body from infection and disease, attacks joint tissues for unknown reasons. White blood cells, the agents of the immune system, travel to the synovium and cause inflammation (synovitis), characterized by warmth, redness, swelling, and pain—typical symptoms of rheumatoid arthritis. During the inflammation process, the normally thin synovium becomes thick and makes the joint swollen puffy, and sometimes warm to the touch.
As rheumatoid arthritis progresses, the inflamed synovium invades and destroys the cartilage and bone within the joint. The surrounding muscles, ligaments, and tendons that support and stabilize the joint become weak and unable to work normally. These effects lead to the pain and joint damage often seen in rheumatoid arthritis. Researchers studying rheumatoid arthritis now believe that it begins to damage bones during the first year or two that a person has the disease, one reason why early diagnosis and treatment are so important.
Some people with rheumatoid arthritis also have symptoms in places other than their joints. Many people with rheumatoid arthritis develop anemia, or a decrease in the production of red blood cells. Other effects that occur less often include neck pain and dry eyes and mouth. Very rarely, people may have inflammation of the blood vessels (vasculitis), the lining of the lungs (pleurisy), or the sac enclosing the heart (pericarditis).

A joint (the place where two bones meet) is surrounded by a capsule that protects and supports it. The joint capsule is lined with a type of tissue called synovium, which produces synovial fluid that lubricates and nourishes joint tissues. In rheumatoid arthritis, the synovium becomes inflamed, causing warmth, redness, swelling, and pain. As the disease progresses, the inflamed synovium invades and damages the cartilage and bone of the joint. Surrounding muscles, ligaments, and tendons become weakened. Rheumatoid arthritis also can cause more generalized bone loss that may lead to osteoporosis (fragile bones that are prone to fracture).
How Does Rheumatoid Arthritis Affect People’s Lives?
Rheumatoid arthritis affects people differently. Some people have mild or moderate forms of the disease, with periods of worsening symptoms, called flares, and periods in which they feel better, called remissions. Others have a severe form of the disease that is active most of the time, lasts for many years or a lifetime, and leads to serious joint damage and disability.
Although rheumatoid arthritis is primarily a disease of the joints, its effects are not just physical. Many people with rheumatoid arthritis also experience issues related to:
- depression, anxiety
- feelings of helplessness
- low self-esteem.
Rheumatoid arthritis can affect virtually every area of a person’s life from work life to family life. It can also interfere with the joys and responsibilities of family life and may affect the decision to have children.
Fortunately, current treatment strategies allow most people with the disease to lead active and productive lives. These strategies include pain-relieving drugs and medications that slow joint damage, a balance between rest and exercise, and patient education and support programs. In recent years, research has led to a new understanding of rheumatoid arthritis and has increased the likelihood that, in time, researchers will find even better ways to treat the disease.
What Causes Rheumatoid Arthritis?
Scientists still do not know exactly what causes the immune system to turn against the body’s own tissues in rheumatoid arthritis, but research over the last few years has begun to piece together the factors involved.
Genetic (inherited) factors: Scientists have discovered that certain genes known to play a role in the immune system are associated with a tendency to develop rheumatoid arthritis. (See “What Research Is Being Conducted on Rheumatoid Arthritis?” for recent genetic developments.) For the genes that have been linked to rheumatoid arthritis, the frequency of the risky gene is only modestly higher in those with rheumatoid arthritis compared with healthy controls. In other words, individual genes by themselves confer only a small relative risk of disease. Some people who have these particular genes never develop the disease. These observations suggest that although a person’s genetic makeup plays an important role in determining if he or she will develop rheumatoid arthritis, it is not the only factor. What is clear, however, is that more than one gene is involved in determining whether a person develops rheumatoid arthritis and how severe the disease will become.
Environmental factors: Many scientists think that something must occur to trigger the disease process in people whose genetic makeup makes them susceptible to rheumatoid arthritis. A variety of factors have been suggested, but a specific agent has not been identified.
Other factors: Some scientists also think that a variety of hormonal factors may be involved. Women are more likely to develop rheumatoid arthritis than men. The disease may improve during pregnancy and flare after pregnancy. Breastfeeding may also aggravate the disease. Contraceptive use may increase a person’s likelihood of developing rheumatoid arthritis. This suggests hormones, or possibly deficiencies or changes in certain hormones, may promote the development of rheumatoid arthritis in a genetically susceptible person who has been exposed to a triggering agent from the environment.
Even though all the answers are not known, one thing is certain: rheumatoid arthritis develops as a result of an interaction of many factors. Researchers are trying to understand these factors and how they work together. (See“What Research Is Being Conducted on Rheumatoid Arthritis?”)
How Is Rheumatoid Arthritis Diagnosed?
Rheumatoid arthritis can be difficult to diagnose in its early stages for several reasons. First, there is no single test for the disease. In addition, symptoms differ from person to person and can be more severe in some people than in others. Also, symptoms can be similar to those of other types of arthritis and joint conditions, and it may take some time for other conditions to be ruled out. Finally, the full range of symptoms develops over time, and only a few symptoms may be present in the early stages. As a result, doctors use a variety of the following tools to diagnose the disease and to rule out other conditions:
Medical history: The doctor begins by asking the patient to describe the symptoms, and when and how the condition started, as well as how the symptoms have changed over time. The doctor will also ask about any other medical problems the patient and close family members have and about any medications the patient is taking. Accurate answers to these questions can help the doctor make a diagnosis and understand the impact the disease has on the patient’s life.
Good communication between patient and doctor is especially important. For example, the patient’s description of pain, stiffness, and joint function and how these change over time is critical to the doctor’s initial assessment of the disease and how it changes over time.
Physical examination: The doctor will check the patient’s reflexes and general health, including muscle strength. The doctor will also examine bothersome joints and observe the patient’s ability to walk, bend, and carry out activities of daily living. The doctor will also look at the skin for a rash and listen to the chest for signs of inflammation in the lungs.
Laboratory tests: A number of lab tests may be useful in confirming a diagnosis of rheumatoid arthritis. Following are some of the more common ones:
- Rheumatoid factor (RF): Rheumatoid factor is an antibody that is present eventually in the blood of most people with rheumatoid arthritis. (An antibody is a special protein made by the immune system that normally helps fight foreign substances in the body.) Not all people with rheumatoid arthritis test positive for rheumatoid factor, and some people test positive for rheumatoid factor, yet never develop the disease. Rheumatoid factor also can be positive in some other diseases; however, a positive RF in a person who has symptoms consistent with those of rheumatoid arthritis can be useful in confirming a diagnosis. Furthermore, high levels of rheumatoid factor are associated with more severe rheumatoid arthritis.
- Anti-CCP antibodies: This blood test detects antibodies to cyclic citrullinated peptide (anti-CCP). This test is positive in most people with rheumatoid arthritis and can even be positive years before rheumatoid arthritis symptoms develop. When used with the RF, this test’s results are very useful in confirming a rheumatoid arthritis diagnosis.
- Others: Other common laboratory tests include a white blood cell count, a blood test for anemia, which is common in rheumatoid arthritis; the erythrocyte sedimentation rate (often called the sed rate), which measures inflammation in the body; and C-reactive protein, another common test for inflammation that is useful both in making a diagnosis and monitoring disease activity and response to anti-inflammatory therapy.
X rays: X rays are used to determine the degree of joint destruction. They are not useful in the early stages of rheumatoid arthritis before bone damage is evident; however, they may be used to rule out other causes of joint pain. They may also be used later to monitor the progression of the disease.
How Is Rheumatoid Arthritis Treated?
Doctors use a variety of approaches to treat rheumatoid arthritis. These are used in different combinations and at different times during the course of the disease and are chosen according to the patient’s individual situation. No matter what treatment the doctor and patient choose, however, the goals are the same: to relieve pain, reduce inflammation, slow down or stop joint damage, and improve the person’s sense of well-being and ability to function.
Good communication between the patient and doctor is necessary for effective treatment. Talking to the doctor can help ensure that exercise and pain management programs are provided as needed, and that drugs are prescribed appropriately. Talking to the doctor can also help people who are making decisions about surgery.
Goals of Treatment
- Relieve pain
- Reduce inflammation
- Slow down or stop joint damage
- Improve a person’s sense of well-being and ability to function.
Current Treatment Approaches
- Lifestyle
- Medications
- Surgery
- Routine monitoring and ongoing care.
Health behavior changes: Certain activities can help improve a person’s ability to function independently and maintain a positive outlook.
- Rest and exercise: People with rheumatoid arthritis need a good balance between rest and exercise, with more rest when the disease is active and more exercise when it is not. Rest helps to reduce active joint inflammation and pain and to fight fatigue. The length of time for rest will vary from person to person, but in general, shorter rest breaks every now and then are more helpful than long times spent in bed.Exercise is important for maintaining healthy and strong muscles, preserving joint mobility, and maintaining flexibility. Exercise can also help people sleep well, reduce pain, maintain a positive attitude, and manage weight. Exercise programs should take into account the person’s physical abilities, limitations, and changing needs.
- Joint care: Some people find using a splint for a short time around a painful joint reduces pain and swelling by supporting the joint and letting it rest. Splints are used mostly on wrists and hands, but also on ankles and feet. A doctor or a physical or occupational therapist can help a person choose a splint and make sure it fits properly. Other ways to reduce stress on joints include self-help devices (for example, zipper pullers, long-handled shoe horns); devices to help with getting on and off chairs, toilet seats, and beds; and changes in the ways that a person carries out daily activities.
- Stress reduction: People with rheumatoid arthritis face emotional challenges as well as physical ones. The emotions they feel because of the disease—fear, anger, and frustration—combined with any pain and physical limitations can increase their stress level. Although there is no evidence that stress plays a role in causing rheumatoid arthritis, it can make living with the disease difficult at times. Stress also may affect the amount of pain a person feels. There are a number of successful techniques for coping with stress. Regular rest periods can help, as can relaxation, distraction, or visualization exercises. Exercise programs, participation in support groups, and good communication with the health care team are other ways to reduce stress.
- Healthful diet: With the exception of several specific types of oils, there is no scientific evidence that any specific food or nutrient helps or harms people with rheumatoid arthritis. However, an overall nutritious diet with enough—but not an excess of—calories, protein, and calcium is important. Some people may need to be careful about drinking alcoholic beverages because of the medications they take for rheumatoid arthritis. Those taking methotrexate may need to avoid alcohol altogether because one of the most serious long-term side effects of methotrexate is liver damage.
- Climate: Some people notice that their arthritis gets worse when there is a sudden change in the weather. However, there is no evidence that a specific climate can prevent or reduce the effects of rheumatoid arthritis. Moving to a new place with a different climate usually does not make a long-term difference in a person’s rheumatoid arthritis.
Medications: Most people who have rheumatoid arthritis take medications.2 Some medications (analgesics) are used only for pain relief; others, such as corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), are used to reduce inflammation.3 Still others, often called disease-modifying antirheumatic drugs (DMARDs), are used to try to slow the course of the disease. Common DMARDs include hydroxychloroquine, leflunomide, methotrexate, and sulfasalazine. Other DMARDs—called biologic response modifiers—may be used in people with more serious disease. These are genetically engineered medications that help reduce inflammation and structural damage to the joints by interrupting the cascade of events that drive inflammation. Currently, several biologic response modifiers are approved for rheumatoid arthritis, including abatacept, adalimumab, anakinra, certolizumab, etanercept, golimumab, infliximab, rituximab, tocilizumab, and tofacitinib. They work in one of several ways:
- Etanercept, golimumab, infliximab, adalimumab and certolizumab, reduce inflammation by blocking tumor necrosis factor (TNF), a cytokine or immune system protein that triggers inflammation during normal immune responses.
- Anakinra works by blocking a cytokine called interleukin-1 (IL-1) that is seen in excess in people with rheumatoid arthritis.
- Rituximab stops the activation of a type of white blood cell called B cells. This reduces the overall activity of the immune system, which is overactive in people with rheumatoid arthritis.
- Abatacept blocks a particular chemical that triggers the overproduction of white blood cells called T cells that play a role in rheumatoid arthritis inflammation.
- Tocilizumab works by blocking a cytokine called interleukin 6 (IL-6) to reduce inflammation in people with rheumatoid arthritis,
Another DMARD, tofacitinib, from a new class of drugs call jak kinase (JAK) inhibitors, fights inflammation from inside the cell to reduce inflammation in people with rheumatoid arthritis.
2All medicines can have side effects. Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
3 Warning: Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other drugs cannot be taken when a patient is being treated with NSAIDs, because NSAIDs alter the way the body uses or eliminates these other drugs. Check with your health care provider or pharmacist before you take NSAIDs. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
For many years, doctors initially prescribed aspirin or other pain-relieving drugs for rheumatoid arthritis, and waited to prescribe more powerful drugs only if the disease worsened. In recent decades this approach to treatment has changed as studies have shown that early treatment with more powerful drugs—and the use of drug combinations instead of one medication alone—may be more effective in reducing or preventing joint damage. Someone with persistent rheumatoid arthritis symptoms should see a doctor familiar with the disease and its treatment to reduce the risk of damage.
The person’s general condition, the current and predicted severity of the illness, the length of time he or she will take the drug, and the drug’s effectiveness and potential side effects are important considerations in prescribing drugs for rheumatoid arthritis.
Many of the drugs that help reduce disease in rheumatoid arthritis do so by reducing the inflammation that can cause pain and joint damage. However, in some instances, inflammation is one mechanism the body normally uses to maintain health, such as to fight infection and possibly to stop tumors from growing. The magnitude of the risk from the treatment is hard to judge because infections and cancer can occur in people with rheumatoid arthritis who are not on treatment, and probably more commonly than in healthy individuals. Nevertheless, appropriate caution and vigilance are justified.
Surgery: Several types of surgery are available to patients with severe joint damage. The primary purpose of these procedures is to reduce pain, improve the affected joint’s function, and improve the patient’s ability to perform daily activities. Surgery is not for everyone, however, and the decision should be made only after careful consideration by the patient and doctor. Together they should discuss the patient’s overall health, the condition of the joint or tendon that will be operated on, and the reason for, as well as the risks and benefits of, the surgical procedure. Cost may be another factor.
Following are some of the more common surgeries performed for rheumatoid arthritis:
- Joint replacement: Joint replacement involves removing all or part of a damaged joint and replacing it with synthetic components. Joint replacement is available for a number of different joints, but the most commonly replaced joints are the hips and knees. Joint replacement surgery is done primarily to relieve pain and improve or preserve function.Although joint replacement traditionally involved a large incision and long recovery, new minimally invasive surgeries are making it possible to do some forms of joint replacement with smaller incisions and a shorter, easier recovery.Artificial joints are not always permanent and may eventually have to be replaced. This may be an important consideration for young people.
- Arthrodesis (fusion): Arthrodesis is a surgical procedure that involves removing the joint and fusing the bones into one immobile unit, often using bone grafts from the person’s own pelvis. Although the procedure limits movement, it can be useful for increasing stability and relieving pain in affected joints. The most commonly fused joints are the ankles and wrists and joints of the fingers and toes.
- Tendon reconstruction: Rheumatoid arthritis can damage and even rupture tendons, the tissues that attach muscle to bone. This surgery, which is used most frequently on the hands, reconstructs the damaged tendon by attaching an intact tendon to it. This procedure can help to restore hand function, especially if the tendon is completely ruptured.
- Synovectomy: In this surgery, the doctor actually removes the inflamed synovial tissue. Synovectomy by itself is seldom performed now because not all of the tissue can be removed, and it eventually grows back. Synovectomy is done as part of reconstructive surgery, especially tendon reconstruction.
Routine monitoring and ongoing care: Regular medical care is important to monitor the course of the disease, determine the effectiveness and any negative effects of medications, and change therapies as needed.
Monitoring typically includes regular visits to the doctor. It also may include blood, urine, and other laboratory tests and x rays.
People with rheumatoid arthritis may want to discuss preventing osteoporosis with their doctors as part of their long-term, ongoing care. Osteoporosis is a condition in which bones become weakened and fragile. Having rheumatoid arthritis increases the risk of developing osteoporosis for both men and women, particularly if a person takes corticosteroids. Such patients may want to discuss with their doctors the potential benefits of calcium and vitamin D supplements or other treatments for osteoporosis.
Alternative and complementary therapies: Special diets, vitamin supplements, and other alternative approaches have been suggested for treating rheumatoid arthritis.
Research shows that some of these, for example, fish oil supplements, may help reduce arthritis inflammation. For most, however, controlled scientific studies either have not been conducted on them or have found no definite benefit to these therapies.
As with any therapy, patients should discuss the benefits and drawbacks with their doctors before beginning an alternative or new type of therapy. If the doctor feels the approach has value and will not be harmful, it can be incorporated into a person’s treatment plan. However, it is important not to neglect regular health care.
Who Treats Rheumatoid Arthritis?
Diagnosing and treating rheumatoid arthritis requires a team effort involving the patient and several types of health care professionals.
The primary doctor to treat arthritis may be an internist, a doctor who specializes in the diagnosis and medical treatment of adults, or a rheumatologist, a doctor who specializes in arthritis and other diseases of the bones, joints, and muscles.
As treatment progresses, other professionals often help. These may include the following:
- Orthopaedists: Surgeons who specialize in the treatment of, and surgery for, bone and joint diseases.
- Physical therapists: Health professionals who work with patients to improve joint function.
- Occupational therapists: Health professionals who teach ways to protect joints, minimize pain, perform activities of daily living, and conserve energy.
- Dietitians: Health professionals who teach ways to use a good diet to improve health and maintain a healthy weight.
- Nurse educators: Nurses who specialize in helping patients understand their overall condition and implement their treatment plans.
- Psychologists: Health professionals who seek to help patients cope with difficulties in the home and workplace that may result from their medical conditions.
What You Can Do: The Importance of Self-Care
Although health care professionals can prescribe or recommend treatments to help patients manage their rheumatoid arthritis, the real key to living well with the disease lies with the patients themselves. Research shows that people who take part in their own care report less pain and make fewer doctor visits. They also enjoy a better quality of life.
Self-management programs teach about rheumatoid arthritis and its treatments, exercise and relaxation approaches, communication between patients and health care providers, and problem solving. Research on these programs has shown that they help people:
- understand the disease
- reduce their pain while remaining active
- cope physically, emotionally, and mentally
- feel greater control over the disease and build a sense of confidence in the ability to function and lead full, active, and independent lives.
What Research Is Being Conducted on Rheumatoid Arthritis?
Over the last several decades, research has greatly increased our understanding of the immune system, genetics, and biology. This research is now showing results in several areas important to rheumatoid arthritis. Scientists are thinking about rheumatoid arthritis in exciting ways that were not possible even 10 years ago.
The National Institutes of Health (NIH) funds a wide variety of medical research at its headquarters in Bethesda, MD, and at universities and medical centers across the United States. One of the NIH institutes, the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), is a major supporter of research and research training in rheumatoid arthritis through grants to individual scientists, Specialized Centers of Research, Multidisciplinary Clinical Research Centers, and Multipurpose Arthritis and Musculoskeletal Diseases Centers.
Following are examples of research in rheumatoid arthritis supported by the Federal Government through the NIAMS and other parts of NIH.
Genetics
Researchers are studying genetic factors that predispose some people to developing rheumatoid arthritis, as well as factors connected with disease severity. Over the past decade, NIAMS-supported research in this area has led to several important genetic discoveries including the following:
Variation in a gene involved in controlling T-cell activation doubles rheumatoid arthritis risk: The variation—called a single nucleotide polymorphism (SNP)—is located within a gene that codes for PTPN22, an enzyme known to be involved in controlling the activation of white blood cells called T cells that play an important role in the body’s immune system. Where the SNP is present in one or both copies of a person’s genes for this enzyme, T cells and other immune cells respond too vigorously, causing increased inflammation and tissue damage. Scientists say the implications of this finding go beyond a better understanding of rheumatoid arthritis risk; it may also help explain why different autoimmune diseases tend to run in families. Other studies have the same SNP with type-1 diabetes and juvenile arthritis.
Genetic variation increases risk of rheumatoid arthritis and lupus: Separate research found a SNP in a large segment of the STAT4 gene increases the risk of both rheumatoid arthritis and another autoimmune disease, systemic lupus erythematosus (lupus). The STAT4 gene encodes a protein that plays an important role in the regulation and activation of certain cells of the immune system. One variant form of the gene was present at a significantly higher frequency in rheumatoid arthritis patient samples from the North American Rheumatoid Arthritis Consortium (NARAC)—a consortium formed to collect, analyze, and make available clinical and genetic data on 1,000 sibling pairs with rheumatoid arthritis—as compared with controls. Scientists replicated that result in two independent collections of rheumatoid arthritis cases and controls.
Twin study shows genetic differences in rheumatoid arthritis: Because identical twins have the exact same genes at conception, scientists believe that changes in the genes after the genome is constructed may account for why one of a twin pair can have rheumatoid arthritis while the other does not. To better understand what those changes might be, scientists have used a sophisticated technique called microarray to examine the expression of more than 20,000 genes at a time in 11 pairs of disease-discordant identical twins (meaning one twin had the disease, the other did not). The examination led to the detection of differences in expression of 827 genes. The most significantly overexpressed gene was laeverin, an enzyme that breaks down certain types of proteins; second was 11ß-hydroxysteroid dehydrogenase type 2 (11ß-HSD2), important in a steroid pathway linked to inflammation and bone erosion; and third was cysteine-rich angiogenic inducer 61 (Cyr61), which is known for its role in angiogenesis, the formation of new blood vessels. The scientists say their findings are exciting because they offer new insights into the mechanisms by which rheumatoid arthritis is mediated.
Genetic region associated with rheumatoid arthritis risk: Using the relatively new genome-wide association approach, which makes it possible to analyze between 300,000 and 500,000 single nucleotide polymorphisms, researchers in the United States and Sweden identified a region of chromosome 9 containing two genes relevant to chronic inflammation: TRAF1 (encoding tumor necrosis factor receptor-associated factor 1) and C5 (encoding complement component 5). Scientists say it is not yet known how the genes in the TRAF1-C5 region influence rheumatoid arthritis risk, but they hope that by learning more about the genes and their role in the disease, they may find clues to influencing treatment of the disease.
Rare gene variants associated with rheumatoid arthritis: Another genome-wide association scan was used to determine that rare variants of a gene that encodes the enzyme sialic acid acetylesterase (SIAE) are associated with several autoimmune diseases, especially rheumatoid arthritis and type 1 diabetes. This discovery suggests that SIAE plays an important role in autoimmunity. They also highlight the promise that rare variant analysis holds for unraveling complex, multigene diseases.
New Therapies
Researchers continue to identify molecules that appear to play a role in rheumatoid arthritis and thus are potential targets for new treatments. The path between identifying the molecule and developing a drug that targets it is long and difficult. Fortunately, this path has been successfully negotiated and new drugs have emerged that successfully reduce symptoms and damage in rheumatoid arthritis. Researchers continue to identify more candidate drugs, with hopes that these will have fewer side effects or will cure more patients.
Tofacitinib, approved for the treatment of rheumatoid arthritis in 2012, is from a new class of drugs developed to target Janus kinases. One member of this family, JAK3, was discovered in the early 1990s by a National Institutes of Health laboratory in the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). Subsequent studies carried out at the National Heart, Lung, and Blood Institute (NHLBI), in collaboration with the NIAMS, showed that genetic defects in JAK3 can cause severe combined immunodeficiency. This discovery led to the idea that drugs blocking Janus kinases would suppress the immune system and might be protective against the damaging inflammation of rheumatoid arthritis and certain other autoimmune diseases.
Understanding Joint Destruction
Advances in understanding the processes that lead to joint destruction are bringing NIAMS-supported researchers a step closer to new therapies to stop the destructive process. In one such study, researchers found a factor they suspect plays a crucial role in joint destruction: an adhesion molecule on cells of the synovium called cadherin-11. Adhesion molecules allow individual cells to stick together to form tissues. At normal levels, cadherin-11 enables the cells (synoviocytes) to adhere together to form the lining layer of the synovium. But when overgrowth of the synovium occurs, cadherin plays a key role in the destructive behavior of the synovium; namely, eroding the cartilage, which causes permanent destruction to the joint. In studies of mice prone to a disease similar to human rheumatoid arthritis, blocking cadherin-11 prevented cartilage destruction. The next step is to determine whether an agent to block an excess of the molecule has the same beneficial effect in people with rheumatoid arthritis.
In other research, scientists found that a lack of apoptosis (programmed cell death) contributes to a proliferation of cells in the joint lining and the failure to eliminate immune cells that react against self. In animal studies, mice lacking two proteins that mediate the process of apoptosis developed arthritis.
Other NIAMS-funded research has led to a better understanding of autoantibodies and how they cause joint damage. Studying the joints of patients with rheumatoid arthritis, researchers found that anti-CCP and rheumatoid factor antibodies from the joints actually bound to a lot of products associated with joint cartilage and also to histones, intracellular proteins from the cell nucleus that associate with DNA in the formation of chromosomes. The histone deposits may be derived from cells that died and spilled their contents, a result of the disease condition. Furthermore, they found that cartilage in RA is actually coated with histones, regardless of whether RA was active or not. Cartilage from joints of people with osteoarthritis (OA) were not covered in histones. The researchers hypothesize that histones on the cartilage bind with antihistone antibodies, contributing to joint-damaging inflammation in rheumatoid arthritis.
Preventing Related Problems
Having rheumatoid arthritis does not make people immune to other medical problems. Thus, reducing the risk of problems that can be associated with rheumatoid arthritis is a focus of NIAMS research. One recent study showed that treatment with hydroxychloroquine, a medication used to treat rheumatic diseases and malaria, reduced the incidence of diabetes in people with rheumatoid arthritis. People with rheumatoid arthritis who took the medication for more than 4 years showed a reduction in risk of diabetes of up to 77 percent.
Bursitis and Tendinitis
This publication contains general information about bursitis and tendinitis. It describes what these conditions are and how they are diagnosed and treated. At the end is a list of key words to help you understand the medical terms used in this publication. If you have further questions after reading this publication, you may wish to discuss them with your doctor.
What Is Bursitis and What Is Tendinitis?
Bursitis and tendinitis are both common conditions that involve inflammation of the soft tissue around muscles and bones, most often in the shoulder, elbow, wrist, hip, knee, or ankle.
A bursa is a small, fluid-filled sac that acts as a cushion between a bone and other moving parts: muscles, tendons, or skin. Bursae are found throughout the body. Bursitis occurs when a bursa becomes inflamed (redness and increased fluid in the bursa).
A tendon is a flexible band of fibrous tissue that connects muscles to bones. Tendinitis is inflammation of a tendon. Tendons transmit the pull of the muscle to the bone to cause movement. They are found throughout the body, including the hands, wrists, elbows, shoulders, hips, knees, ankles, and feet. Tendons can be small, like those found in the hand, or large, like the Achilles tendon in the heel.
- What Causes These Conditions?
- What Parts of the Body Are Affected?
- How Are These Conditions Diagnosed?
- What Kind of Health Care Professional Treats These Conditions?
- How Are Bursitis and Tendinitis Treated?
- Can Bursitis and Tendinitis Be Prevented?
- What Research Is Being Conducted on Bursitis and Tendonitis?
- Where Can People Find More Information About Bursitis and Tendinitis?
- Key Words
Illustrations
What Causes These Conditions?
Bursitis is commonly caused by overuse or direct trauma to a joint. Bursitis may occur at the knee or elbow, from kneeling or leaning on the elbows longer than usual on a hard surface, for example. Tendinitis is most often the result of a repetitive injury or motion in the affected area. These conditions occur more often with age. Tendons become less flexible with age, and therefore, more prone to injury.
People such as carpenters, gardeners, musicians, and athletes who perform activities that require repetitive motions or place stress on joints are at higher risk for tendinitis and bursitis.
An infection, arthritis, gout, thyroid disease, and diabetes can also bring about inflammation of a bursa or tendon.
What Parts of the Body Are Affected?
Tendinitis causes pain and tenderness just outside a joint. Some common names for tendinitis identify with the sport or movement that typically increases risk for tendon inflammation. They include tennis elbow, golfer’s elbow, pitcher’s shoulder, swimmer’s shoulder, and jumper’s knee. Some common examples follow.
Tennis Elbow and Golfer’s Elbow
Tennis elbow refers to an injury to the outer elbow tendon. Golfer’s elbow is an injury to the inner tendon of the elbow. These conditions can also occur with any activity that involves repetitive wrist turning or hand gripping, such as tool use, hand shaking, or twisting movements. Carpenters, gardeners, painters, musicians, manicurists, and dentists are at higher risk for these forms of tendinitis. Pain occurs near the elbow, sometimes radiating into the upper arm or down to the forearm. Another name for tennis elbow is lateral epicondylitis. Golfer’s elbow is also called medial epicondylitis.
Structure of the Elbow (Representation)

Shoulder Tendinitis, Bursitis, and Impingement Syndrome
Two types of tendinitis can affect the shoulder. Biceps tendinitis causes pain in the front or side of the shoulder and may travel down to the elbow and forearm. Pain may also occur when the arm is raised overhead. The biceps muscle, in the front of the upper arm, helps stabilize the upper arm bone (humerus) in the shoulder socket. It also helps accelerate and decelerate the arm during overhead movement in activities like tennis or pitching.
Structure of the Shoulder (Representation)

Rotator cuff tendinitis causes shoulder pain at the tip of the shoulder and the upper, outer arm. The pain can be aggravated by reaching, pushing, pulling, lifting, raising the arm above shoulder level, or lying on the affected side. The rotator cuff is primarily a group of four muscles that attach the arm to the shoulder joint and allow the arm to rotate and elevate. If the rotator cuff and bursa are irritated, inflamed, and swollen, they may become compressed between the head of the humerus and the acromion, the outer edge of the shoulder blade. Repeated motion involving the arms, or the aging process involving shoulder motion over many years, may also irritate and wear down the tendons, muscles, and surrounding structures. Squeezing of the rotator cuff is called shoulder impingement syndrome.
Inflammation caused by rheumatoid arthritis may cause rotator cuff tendinitis and bursitis. Sports involving overuse of the shoulder and occupations requiring frequent overhead reaching are other potential causes of irritation to the rotator cuff or bursa, and may lead to inflammation and impingement.
Knee Tendinitis or Jumper’s Knee
If a person overuses a tendon during activities such as dancing, cycling, or running, it may elongate or undergo microscopic tears and become inflamed. Trying to break a fall may also cause the quadriceps muscles to contract and tear the quadriceps tendon above the knee cap (patella) or the patellar tendon below it. This type of injury is most likely to happen in older people whose tendons tend to be weaker and less flexible. Tendinitis of the patellar tendon is sometimes called jumper’s knee because in sports that require jumping, such as basketball, the muscle contraction and force of hitting the ground after a jump strain the tendon. After repeated stress, the tendon may become inflamed or tear.
Lateral View of the Knee (Representation)

People with tendinitis of the knee may feel pain during running, hurried walking, or jumping. Knee tendinitis can increase risk for ruptures or large tears to the tendon. A complete rupture of the quadriceps or patellar tendon is not only painful, but also makes it difficult for a person to bend, extend, or lift the leg, or to bear weight on the involved leg.
Achilles Tendinitis
Achilles tendon injuries involve an irritation, stretch, or tear to the tendon connecting the calf muscle to the back of the heel. Achilles tendinitis is a common overuse injury, but can also be caused by tight or weak calf muscles or any condition that causes the tendon to become less flexible and more rigid, such as reactive arthritis or normal aging.
Achilles tendon injuries can happen to anyone who regularly participates in an activity that causes the calf muscle to contract, like climbing stairs or using a stair-stepper, but are most common in middle-aged “weekend warriors” who may not exercise regularly. Among professional athletes, most Achilles injuries seem to occur in quick-acceleration or jumping sports like football, tennis, and basketball, and almost always end the season’s competition for the athlete.
Achilles tendinitis can be a chronic condition. It can also cause what appears to be a sudden injury. Tendinitis is the most common factor contributing to Achilles tendon tears. When a tendon is weakened by age or overuse, trauma can cause it to rupture. These injuries can be so sudden and agonizing that they have been known to bring down charging professional football players in shocking fashion.
Lateral View of the Ankle (Representation)

How Are These Conditions Diagnosed?
Diagnosis of tendinitis and bursitis begins with a medical history and physical examination. The patient will describe the pain and circumstances in which pain occurs. The location and onset of pain, whether it varies in severity throughout the day, and the factors that relieve or aggravate the pain are all important diagnostic clues. Therapists and physicians will use manual tests called selective tissue tension tests to determine which tendon is involved, and then will palpate (a form of touching the tendon) specific areas of the tendon to pinpoint the area of inflammation. X rays do not show tendons or bursae, but may be helpful in ruling out bone problems or arthritis. In the case of a torn tendon, x rays may help show which tendon is affected. In a knee injury, for example, an x ray will show that the patella is lower than normal in a quadriceps tendon tear and higher than normal in a patellar tendon tear. The doctor may also use magnetic resonance imaging (MRI) to confirm a partial or total tear. MRIs detect both bone and soft tissues like muscles, tendons and their coverings (sheaths), and bursae.
To rule out infection, the doctor may remove and test fluid from the inflamed area.
What Kind of Health Care Professional Treats These Conditions?
A primary care physician or a physical therapist can treat the common causes of tendinitis and bursitis. Complicated cases or those resistant to conservative therapies may require referral to a specialist, such as an orthopaedist or rheumatologist.
How Are Bursitis and Tendinitis Treated?
Treatment focuses on healing the injured bursa or tendon. The first step in treating both of these conditions is to reduce pain and inflammation with rest, compression, elevation, and anti-inflammatory medicines such as aspirin, naproxen, or ibuprofen. Ice may also be used in acute injuries, but most cases of bursitis or tendinitis are considered chronic, and ice is not helpful. When ice is needed, an ice pack can be applied to the affected area for 15 to 20 minutes every 4 to 6 hours for 3 to 5 days. Longer use of ice and a stretching program may be recommended by a health care provider.
Activity involving the affected joint is also restricted to encourage healing and prevent further injury.
In some cases (e.g., in tennis elbow), elbow bands may be used to compress the forearm muscle to provide some pain relief, limiting the pull of the tendon on the bone. Other protective devices, such as foot orthoses for the ankle and foot or splints for the knee or hand, may temporarily reduce stress to the affected tendon or bursa and facilitate quicker healing times, while allowing general activity levels to continue as usual.
Gentle stretching and strengthening exercises are added gradually. Massage of the soft tissue may be helpful. These may be preceded or followed by use of an ice pack. The type of exercises recommended may vary depending on the location of the affected bursa or tendon.
If there is no improvement, the doctor may inject a corticosteroid medicine into the area surrounding the inflamed bursa or tendon. Although corticosteroid injections are a common treatment, they must be used with caution because they may lead to weakening or rupture of the tendon (especially weight-bearing tendons such as the Achilles [ankle], posterior tibial [arch of the foot], and patellar [knee] tendons). If there is still no improvement after 6 to 12 months, the doctor may perform either arthroscopic or open surgery to repair damage and relieve pressure on the tendons and bursae.
If the bursitis is caused by an infection, the doctor will prescribe antibiotics.
If a tendon is completely torn, surgery may be needed to repair the damage. After surgery on a quadriceps or patellar tendon, for example, the patient will wear a cast or brace or immobilizing device for 3 to 6 weeks and use crutches. For a partial tear, the doctor might apply a cast without performing surgery.
Rehabilitating a partial or complete tear of a tendon requires an exercise program to restore the ability to bend and straighten the knee and to strengthen the leg to prevent repeat injury. A rehabilitation program may last up to 6 months, although the patient can return to many activities before then.
Can Bursitis and Tendinitis Be Prevented?
To help prevent inflammation or reduce the severity of its recurrence:
- Begin new activities or exercise regimens slowly.
- Gradually increase physical demands following several well-tolerated exercise sessions.
- Exercise regularly.
- Strengthen muscles around the joint.
- Take breaks from repetitive tasks often.
- Stop activities that cause pain.
- Cushion the affected joint. Use foam for kneeling or elbow pads. Increase the gripping surface of tools with gloves or padding. Apply grip tape or an oversized grip to golf clubs.
- Use two hands to hold heavy tools; use a two-handed backhand in tennis.
- Don’t sit still for long periods.
- Practice good posture and position the body properly when going about daily activities.
- If a history of tendinitis is present, consider seeking guidance from your doctor or therapist before engaging in new exercises and activities.
Other Resources
American Academy of Orthopaedic Surgeons
Website: http://www.aaos.org
American College of Rheumatology
Website: http://www.rheumatology.org
American Physical Therapy Association
Website: http://www.apta.org
Arthritis Foundation
Website: http://www.arthritis.org
For additional information, visit the NIAMS Web site or call the NIAMS Information Clearinghouse.
Key Words
Acromion. The outer part of the shoulder blade.
Arthroscopic surgery. Repairing the interior of a joint by inserting a microscope-like device and surgical tools through small cuts rather than one, large surgical cut.
Biceps muscle. The muscle in the front of the upper arm.
Bursa. A small sac of tissue located between a bone and other moving structures such as muscles, skin, or tendons. The bursa contains a lubricating fluid that allows these structures to glide smoothly.
Bursitis. Inflammation or irritation of a bursa.
Corticosteroids. Synthetic preparations of cortisol, which is a hormone produced by the body. Corticosteroids block the immune system’s production of substances that trigger allergic and inflammatory responses. These drugs may be injected directly into the inflammation site. Generally, symptoms improve or disappear within several days. Frequent injections into the same site are not recommended.
Epicondylitis. A painful and sometimes disabling swelling of the tissues of the elbow.
Humerus. The upper arm bone.
Impingement syndrome. When the rotator cuff becomes inflamed and thickened, it may get trapped under the acromion, resulting in pain or loss of motion.
Inflammation. The characteristic reaction of tissue to injury or disease. It is marked by four signs: swelling, redness, heat, and pain.
Joint. A junction where two bones meet. Most joints are composed of cartilage, joint space, the fibrous capsule, the synovium, and ligaments.
Muscle. A tissue that has the ability to contract, producing movement or force. There are three types of muscle: striated muscle, which is attached to the skeleton; smooth muscle, which is found in such tissues as the stomach and blood vessels; and cardiac muscle, which forms the walls of the heart. For striated muscle to function at its ideal level, the joint and surrounding structures must all be in good condition.
Patella. A flat triangular bone located at the front of the knee joint. Also called the kneecap.
Quadriceps muscle. The large muscle at the front of the thigh.
Radius. The larger of the two bones in the forearm.
Range of motion. The extent to which a joint can move freely and easily.
Rheumatoid arthritis. An autoimmune inflammatory disease that causes pain, swelling, stiffness, and loss of function in the joints.
Rotator cuff. A set of muscles and tendons that secures the arm to the shoulder blade and permits rotation of the arm.
Tendinitis. Inflammation or irritation of a tendon.
Tendons. Fibrous cords that connect muscle to bone.
What is Peripheral Neuropathy?
An estimated 20 million people in the United States have some form of peripheral neuropathy, a condition that develops as a result of damage to the peripheral nervous system — the vast communications network that transmits information between the central nervous system (the brain and spinal cord) and every other part of the body. (Neuropathy means nerve disease or damage.) Symptoms can range from numbness or tingling, to pricking sensations (paresthesia), or muscle weakness. Areas of the body may become abnormally sensitive leading to an exaggeratedly intense or distorted experience of touch (allodynia). In such cases, pain may occur in response to a stimulus that does not normally provoke pain. Severe symptoms may include burning pain (especially at night), muscle wasting, paralysis, or organ or gland dysfunction. Damage to nerves that supply internal organs may impair digestion, sweating, sexual function, and urination. In the most extreme cases, breathing may become difficult, or organ failure may occur.
Peripheral nerves send sensory information back to the brain and spinal cord, such as a message that the feet are cold. Peripheral nerves also carry signals from the brain and spinal cord to the muscles to generate movement. Damage to the peripheral nervous system interferes with these vital connections. Like static on a telephone line, peripheral neuropathy distorts and sometimes interrupts messages between the brain and spinal cord and the rest of the body.
Peripheral neuropathies can present in a variety of forms and follow different patterns. Symptoms may be experienced over a period of days, weeks, or years. They can be acute or chronic. In acute neuropathies such as Guillain-Barré syndrome (in which the body’s immune system attacks part of the peripheral nervous system and impairs sending and receiving nerve signals), symptoms appear suddenly, progress rapidly, and resolve slowly as damaged nerves heal. In chronic forms, symptoms begin subtly and progress slowly. Some people may have periods of relief followed by relapse. Others may reach a plateau stage where symptoms stay the same for many months or years. Many chronic neuropathies worsen over time. Although neuropathy may be painful and potentially debilitating, very few forms are fatal.
In diabetic neuropathy, one of the most common forms of peripheral neuropathy, nerve damage occurs in an ascending pattern. The first nerve fibers to malfunction are the ones that travel the furthest from the brain and the spinal cord. Pain and numbness often are felt symmetrically in both feet followed by a gradual progression up both legs. Later, the fingers, hands, and arms may become affected.
How are the peripheral neuropathies classified?
More than 100 types of peripheral neuropathy have been identified, each with its own symptoms and prognosis. In general, peripheral neuropathies are classified according to the type of damage to the nerves. Some forms of neuropathy involve damage to only one nerve and are calledmononeuropathies. More frequently however, multiple nerves are affected, called polyneuropathy.
Some peripheral neuropathies are due to damage to the axons (the long, threadlike portion of the nerve cell), while others are due to damage to the myelin sheath, the fatty protein that coats and insulates the axon. Peripheral neuropathies may also be caused by a combination of both axonal damage and demyelination. Electrodiagnostic studies can help healthcare providers determine the type of damage involved.
What are the symptoms of peripheral nerve damage?
Symptoms vary depending on whether motor, sensory, or autonomic nerves are damaged. Motor nerves control voluntary movement of muscles such as those used for walking, grasping things, or talking. Sensory nerves transmit information such as the feeling of a light touch or the pain from a cut. Autonomic nerves control organ activities that are regulated automatically such as breathing, digesting food, and heart and gland functions. Some neuropathies may affect all three types of nerves; others primarily affect one or two types. Doctors may use terms such as predominantly motor neuropathy, predominantly sensory neuropathy, sensory-motor neuropathy, or autonomic neuropathy to describe the types of nerves involved in an individual’s condition.
Motor nerve damage is most commonly associated with muscle weakness. Other symptoms may include painful cramps and fasciculations (uncontrolled muscle twitching visible under the skin), muscle atrophy (severe shrinkage of muscle size), and decreased reflexes.
Sensory nerve damage causes a variety of symptoms because sensory nerves have a broad range of functions. Larger sensory fibers enclosed in myelin register vibration, light touch, and position sense. Damage to large sensory fibers impairs touch, resulting in a general decrease in sensation. Since this is felt most in the hands and feet, people may feel as if they are wearing gloves and stockings even when they are not. This damage to larger sensory fibers may contribute to the loss of reflexes. Loss of position sense often makes people unable to coordinate complex movements like walking or fastening buttons, or to maintain their balance when their eyes are shut.
Smaller sensory fibers without myelin sheaths transmit pain and temperature sensations. Damage to these fibers can interfere with the ability to feel pain or changes in temperature. People may fail to sense that they have been injured from a cut or that a wound is becoming infected. Others may not detect pain that warns of impending heart attack or other acute conditions. Loss of pain sensation is a particularly serious problem for people with diabetes, contributing to the high rate of lower limb amputations among this population.
Neuropathic pain is a common, often difficult to control symptom of sensory nerve damage and can seriously affect emotional well-being and overall quality of life. Often worse at night, neuropathic pain seriously disrupts sleep and adds to the emotional burden of sensory nerve damage. Neuropathic pain can often be associated with an oversensitization of pain receptors in the skin, so that people feel severe pain (allodynia) from stimuli that are normally painless. For example, some may experience pain from bed sheets draped lightly over the body. Over many years, sensory neuropathy may lead to changes in the skin, hair, as well as to joint and bone damage. Unrecognized injuries due to poor sensation contribute to these changes, so it is important for people with neuropathy to inspect numb areas for injury or damage.
Autonomic nerve damage symptoms are diverse since the parasympathetic and sympathetic nerves of the peripheral nervous system control nearly every organ in the body. Common symptoms of autonomic nerve damage include an inability to sweat normally, which may lead to heat intolerance; a loss of bladder control; and an inability to control muscles that expand or contract blood vessels to regulate blood pressure. A drop in blood pressure when a person moves suddenly from a seated to a standing position (a condition known as postural or orthostatic hypotension) may result in dizziness, lightheadedness, or fainting. Irregular heartbeats may also occur.
Gastrointestinal symptoms may accompany autonomic neuropathy. Malfunction of nerves controlling intestinal muscle contractions can lead to diarrhea, constipation, or incontinence. Many people also have problems eating or swallowing if autonomic nerves controlling these functions are affected.
What causes peripheral neuropathy?
Peripheral neuropathy may be either inherited or acquired through disease processes or trauma. In many cases, however, a specific cause cannot be identified. Doctors usually refer to neuropathies with no known cause as idiopathic.
Causes of acquired peripheral neuropathy include:
Physical injury (trauma) is the most common cause of acquired nerve injury.
- Injury or sudden trauma, such as from automobile accidents, falls, sports-related activities, and surgical procedures can cause nerves to be partially or completely severed, crushed, compressed, or stretched, sometimes so forcefully that they are partially or completely detached from the spinal cord. Less severe traumas also can cause serious nerve damage. Broken or dislocated bones can exert damaging pressure on neighboring nerves.
- Repetitive stress frequently leads to entrapment neuropathies, a form of compression injury. Cumulative damage can result from repetitive, awkward, and/or forceful activities that require movement of any group of joints for prolonged periods. The resulting irritation may cause ligaments, tendons, and muscles to become inflamed and swollen, constricting the narrow passageways through which some nerves pass. Ulnar neuropathy and carpal tunnel syndrome are examples of the most common types of neuropathy from trapped or compressed nerves at the elbow or wrist.
Diseases or disorders and their related processes (such as inflammation) can be associated with peripheral neuropathy.
- Metabolic and endocrine disorders impair the body’s ability to transform nutrients into energy and process waste products, and this can lead to nerve damage. Diabetes mellitus, characterized by chronically high blood glucose levels, is a leading cause of peripheral neuropathy in the United States. About 60 percent to 70 percent of people with diabetes have mild to severe forms of nervous system damage that can affect sensory, motor, and autonomic nerves and present with varied symptoms. Some metabolic liver diseases also lead to neuropathies as a result of chemical imbalances. Endocrine disorders that lead to hormonal imbalances can disturb normal metabolic processes and cause neuropathies. For example, an underproduction of thyroid hormones slows metabolism, leading to fluid retention and swollen tissues that can exert pressure on peripheral nerves. Overproduction of growth hormone can lead to acromegaly, a condition characterized by the abnormal enlargement of many parts of the skeleton, including the joints. Nerves running through these affected joints often become entrapped, causing pain.
- Small vessel disease can decrease oxygen supply to the peripheral nerves and lead to serious nerve tissue damage. Diabetes frequently leads to impaired blood flow to nerves. Various forms of vasculitis (blood vessel inflammation) frequently cause vessel walls to harden, thicken, and develop scar tissue, decreasing their diameter and impeding blood flow. Vasculitis is an example of nerve damage called mononeuritis multiplex or multifocal mononeuropathy, in which isolated nerves in two or more areas are damaged.
- Autoimmune diseases, in which the immune system attacks the body’s own tissues, can lead to nerve damage. Sjogren’s syndrome, lupus, and rheumatoid arthritis are among the autoimmune diseases that can be associated with peripheral neuropathy. When the tissue surrounding nerves becomes inflamed, the inflammation can spread directly into nerve fibers. Over time, these chronic autoimmune conditions can destroy joints, organs, and connective tissues, making nerve fibers more vulnerable to compression injuries and entrapment. Chronic conditions may alternate between remission and relapse. Acute inflammatory demyelinating neuropathy, better known as Guillain- Barré syndrome, can damage motor, sensory, and autonomic nerve fibers.Most people recover from this autoimmune syndrome although severe cases can be life threatening. Chronic inflammatory demyelinating polyneuropathy (CIDP) usually damages sensory and motor nerves, leaving autonomic nerves intact. Multifocal motor neuropathy is a form of inflammatory neuropathy that affects motor nerves exclusively. It may be chronic or acute.
- Kidney disorders may cause neuropathies. Kidney dysfunction can lead to abnormally high amounts of toxic substances in the blood that can damage nerve tissue. A majority of indviduals who require dialysis because of kidney failure develop polyneuropathy.
- Cancers can infiltrate nerve fibers or exert damaging compression forces on nerve fibers. Tumors also can arise directly from nerve tissue cells. Paraneoplastic syndromes, a group of rare degenerative disorders that are triggered by a person’s immune system response to a cancerous tumor, also can indirectly cause widespread nerve damage. Toxicity from the chemotherapeutic agents and radiation used to treat cancer also can cause peripheral neuropathy. An estimated 30 to 40 percent of people who undergo chemotherapy develop peripheral neuropathy and it is a leading reason why people with cancer stop chemotherapy early. The severity of chemotherapyinduced peripheral neuropathy (CIPN) varies from person to person. In some cases people may be able to ease their symptoms by lowering their chemotherapy dose or by stopping it temporarily. In others, CIPN may persist long after stopping chemotherapy.
- Neuromas are benign tumors that are caused by an overgrowth of nerve tissue that develops after a penetrating injury that severs nerve fibers. Neuromas are often associated with intense pain and sometimes they engulf neighboring nerves, leading to further damage and even greater pain. Neuroma formation can be one element of a more widespread neuropathic pain condition called complex regional pain syndrome or reflex sympathetic dystrophy syndrome, which can be caused by traumatic injuries or surgical trauma. Widespread polyneuropathy is often associated with neurofibromatosis, a genetic disorder in which multiple benign tumors grow on nerve tissue.
- Infections can cause peripheral neuropathy. Viruses and bacteria that can attack nerve tissues include herpes varicellazoster (shingles), Epstein-Barr virus, West Nile virus, cytomegalovirus, and herpes simplex members of the large family of human herpes viruses. These viruses can severely damage sensory nerves, causing attacks of sharp, lightning-like pain. Postherpetic neuralgia is long-lasting, particularly intense pain that often occurs after an attack of shingles. Lyme disease, diphtheria, and leprosy are bacterial diseases characterized by extensive peripheral nerve damage. Diphtheria and leprosy are rare in the United States, but the incidence of Lyme disease is on the rise.The tick-borne infection can involve a wide range of neuropathic disorders, including a rapidly developing, painful polyneuropathy, often within a few weeks of being infected. West Nile virus is spread by mosquitoes and is associated with a severe motor neuropathy. The inflammation triggered by infection sometimes results in various forms of inflammatory neuropathies that develop quickly or slowly.The human immunodeficiency virus (HIV) that causes AIDS is associated with several different forms of neuropathy, depending on the nerves affected and the specific stage of active immunodeficiency disease. A rapidly progressive, painful polyneuropathy affecting the feet and hands can be the first clinically apparent symptom of HIV infection. An estimated 30 percent of people who are HIV positive develop peripheral neuropathy; 20 percent develop distal neuropathic pain.
Exposure to toxins may damage nerves and cause peripheral neuropathy.
- Medication toxicity can be caused by many agents in addition to those for fighting cancer. Other agents that commonly cause peripheral neuropathy as a side effect include those used to fight infection such as antiretroviral agents for treating HIV. In addition, anticonvulsant agents and some heart and blood pressure medications can commonly cause peripheral neuropathy. In most cases, the neuropathy resolves when these medications are discontinued or dosages are adjusted.
- Environmental or industrial toxins such as lead, mercury, and arsenic can cause peripheral neuropathy. In addition, certain insecticides and solvents have also been known to cause neuropathies.
- Heavy alcohol consumption is a common cause of peripheral neuropathy. Damage to the nerves associated with long-term alcohol abuse may not be reversible when a person stops drinking alcohol, however, doing so may provide some symptom relief and prevent further damage. Chronic alcohol abuse also frequently leads to nutritional deficiencies (including B12, thiamine, and folate) that contribute to the development of peripheral neuropathy.
Genetic mutations can either be inherited or arise de novo, meaning they are completely new mutations to an individual and are not passed along by either parent. Some genetic mutations lead to mild neuropathies with symptoms that begin in early adulthood and result in little, if any, significant impairment. More severe hereditary neuropathies often appear in infancy or childhood.
Advances in genetic testing in the last decade have led to significant strides in the ability to identify the genetic causes underlying peripheral neuropathies. For example, several genes have been found to play a role in different types of Charcot-Marie-Tooth, a group of disorders that are among the most common forms of inherited peripheral neuropathies. These neuropathies result from mutations in genes responsible for maintaining the health of the myelin sheath as well as the axons themselves. Key characteristics of Charcot- Marie-Tooth disorders include extreme weakening and wasting of muscles in the lower legs and feet, gait abnormalities, loss of tendon reflexes, and numbness in the lower limbs.
How is peripheral neuropathy diagnosed?
The symptoms of peripheral neuropathy are highly variable. A thorough neurological examination is required to sort out the cause of the symptoms and involves taking an extensive medical history (covering symptoms, work environment, social habits, exposure to toxins, alcohol use, risk of HIV or other infectious diseases, and family history of neurological diseases). In addition, tests are usually performed to identify the cause of the neuropathy as well as the extent and type of nerve damage.
A physical examination and various tests may reveal the presence of a systemic disease causing the nerve damage. Tests of muscle strength, as well as evidence of cramps or fasciculations, indicate motor fiber involvement. Evaluation of the person’s ability to sense vibration, light touch, body position, temperature, and pain reveals any sensory nerve damage and may indicate whether small or large sensory nerve fibers are affected.
Blood tests can detect diabetes, vitamin deficiencies, liver or kidney dysfunction, other metabolic disorders, and signs of abnormal immune system activity. An examination of cerebrospinal fluid that surrounds the brain and spinal cord can reveal abnormal antibodies associated with some immune-mediated neuropathies. More specialized tests may reveal other blood or cardiovascular diseases, connective tissue disorders, or malignancies. Genetic tests are becoming available for a number of the inherited neuropathies.
Based on the results of the neurological exam, physical exam, patient history, and any previous screening or testing, the following additional tests may be ordered to help determine the nature and extent of the neuropathy:
- Nerve conduction velocity (NCV) tests can measure the degree of damage in large nerve fibers, revealing whether symptoms are caused by degeneration of the myelin sheath or the axon. The myelin covering is responsible for the very fast speed of nerve conduction. During this test, a probe electrically stimulates a nerve fiber, which responds by generating its own electrical impulse. An electrode placed further along the nerve’s pathway measures the speed of impulse transmission along the axon. Slow transmission rates and impulse blockage tend to indicate damage to the myelin sheath, while a reduction in the strength of impulses at normal speeds is a sign of axonal degeneration.
- Electromyography (EMG) involves inserting a fine needle into a muscle to record electrical activity when muscles are at rest and when they contract. EMG tests detect abnormal electrical activity in motor neuropathy and can help differentiate between muscle and nerve disorders.
- Magnetic resonance imaging (MRI) can show muscle quality and size, detect fatty replacement of muscle tissue, and can help rule out tumors, herniated discs, or other abnormalities that may be causing the neuropathy.
- Nerve biopsy involves removing and examining a sample of nerve tissue, most often from the lower leg. Although this test can provide valuable information about the degree of nerve damage, it is an invasive procedure that is difficult to perform and may itself cause neuropathic side effects.
- Skin biopsy is a test in which doctors remove a thin skin sample and examine nerve fiber endings. This test offers some unique advantages over NCV tests and nerve biopsy. Unlike NCV, it can reveal damage present in smaller fibers; in contrast to conventional nerve biopsy, skin biopsy is less invasive, has fewer side effects, and is easier to perform.
What treatments are available?
Address underlying conditions
The first step in treating peripheral neuropathy is to address any contributing causes such as infection, toxin exposure, medication-related toxicity, vitamin deficiencies, hormonal deficiencies, autoimmune disorders, or compression that can lead to neuropathy. Peripheral nerves have the ability to regenerate axons, as long as the nerve cell itself has not died, which may lead to functional recovery over time. Correcting an underlying condition often can result in the neuropathy resolving on its own as the nerves recover or regenerate.
The adoption of healthy lifestyle habits such as maintaining optimal weight, avoiding exposure to toxins, exercising, eating a balanced diet, correcting vitamin deficiencies, and limiting or avoiding alcohol consumption can reduce the effects of peripheral neuropathy. Exercise can reduce cramps, improve muscle strength, and prevent muscle wasting. Various dietary strategies can improve gastrointestinal symptoms. Timely treatment of injuries can help prevent permanent damage. Smoking cessation is particularly important because smoking constricts the blood vessels that supply nutrients to the peripheral nerves and can worsen neuropathic symptoms. Self-care skills such as meticulous foot care and careful wound treatment in people with diabetes and others who have an impaired ability to feel pain can alleviate symptoms and improve quality of life. Such changes often create conditions that encourage nerve regeneration.
Systemic diseases frequently require more complex treatments. Strict control of blood glucose levels has been shown to reduce neuropathic symptoms and help people with diabetic neuropathy avoid further nerve damage.
Inflammatory and autoimmune conditions leading to neuropathy can be controlled in several ways. Immunosuppressive drugs such as prednisone, cyclosporine, or azathioprine may be beneficial. Plasmapheresis — a procedure in which blood is removed, cleansed of immune system cells and antibodies, and then returned to the body — can help reduce inflammation or suppress immune system activity. Large intravenously administered doses of immunoglobulins (antibodies that alter the immune system, and agents such as rituximab that target specific inflammatory cells) also can suppress abnormal immune system activity.
Symptom Management
Neuropathic pain, or pain caused by the injury to a nerve or nerves, is often difficult to control. Mild pain may sometimes be alleviated by over-the-counter analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs). More chronic and discomforting pain may need to be addressed through the care of a physician. Medications that are used for chronic neuropathic pain fall under several classes of drugs: antidepressants, anticonvulsant medications, antiarrythmic medications, and narcotic agents. The antidepressant and anticonvulsant medications modulate pain through their mechanism of action on the peripheral nerves, spinal cord, or brain and tend to be the most effective types of medications to control neuropathic pain. Antidepressant medications include tricyclic antidepressants such as amitriptyline or newer serotonin-norepinephrine reuptake inhibitors such as duloxetine hydrochloride or venlafaxine. Anticonvulsant medications that are frequently used include gabapentin, pregabalin, topiramate, and carbamazepine, although other medications used for treating epilepsy may also be useful. Mexiletine is an antiarrythmic medication that may be used for treatment of chronic painful neuropathies.
For pain that does not respond to the previously described medications, the addition of narcotic agents may be considered. Because the use of prescriptionobtained pain relievers that contain opioids can lead to dependence and addiction, their use is recommended only after other means of controlling the pain have failed. One of the newest narcotic medications approved for the treatment of diabetic neuropathy is tapentadol, a drug with both opioid activity and norepinephrine-reuptake inhibition activity of an antidepressant.
Topically administered medications are another option for neuropathic pain. Two agents are topical lidocaine, an anesthetic agent, and capsaicin, a substance found in hot peppers that modifies peripheral pain receptors. Topical agents are generally most appropriate for localized chronic pain such as herpes zoster neuralgia (shingles) pain. Their usefulness for treating diffuse chronic diabetic neuropathy is more limited.
Transcutaneous electrical nerve stimulation (TENS) is a non-invasive intervention used for pain relief in a range of conditions, and a number of studies have described its use for neuropathic pain. The therapy involves attaching electrodes to the skin at the site of pain or near associated nerves and then administering a gentle electrical current. Although data from controlled clinical trials are not available to broadly establish its efficacy for peripheral neuropathies, TENS has been shown in some studies to improve peripheral neuropathy symptoms associated with diabetes.
Other complementary approaches may provide additional support and pain relief. For example, mechanical aids such as hand or foot braces can help reduce pain and physical disability by compensating for muscle weakness or alleviating nerve compression. Orthopedic shoes can improve gait disturbances and help prevent foot injuries in people with a loss of pain sensation. Acupuncture, massage, and herbal medications also are considered in the treatment of neuropathic pain.
Surgical intervention can be considered for some types of neuropathies. Injuries to a single nerve caused by focal compression such as at the carpal tunnel of the wrist, or other entrapment neuropathies, may respond well to surgery that releases the nerve from the tissues compressing it. Some surgical procedures reduce pain by destroying the nerve; this approach is appropriate only for pain caused by a single nerve and when other forms of treatment have failed to provide relief. Peripheral neuropathies that involve more diffuse nerve damage, such as diabetic neuropathy, are not amenable to surgical intervention.
What is Trigeminal Neuralgia?
Trigeminal neuralgia (TN), also called tic douloureux, is a chronic pain condition that causes extreme, sporadic, sudden burning or shock-like face pain. The pain seldom lasts more than a few seconds or a minute or two per episode. The intensity of pain can be physically and mentally incapacitating. TN pain is typically felt on one side of the jaw or cheek. Episodes can last for days, weeks, or months at a time and then disappear for months or years. In the days before an episode begins, some patients may experience a tingling or numbing sensation or a somewhat constant and aching pain. The attacks often worsen over time, with fewer and shorter pain-free periods before they recur. The intense flashes of pain can be triggered by vibration or contact with the cheek (such as when shaving, washing the face, or applying makeup), brushing teeth, eating, drinking, talking, or being exposed to the wind. TN occurs most often in people over age 50, but it can occur at any age, and is more common in women than in men. There is some evidence that the disorder runs in families, perhaps because of an inherited pattern of blood vessel formation. Although sometimes debilitating, the disorder is not life-threatening.
The presumed cause of TN is a blood vessel pressing on the trigeminal nerve in the head as it exits the brainstem. TN may be part of the normal aging process but in some cases it is the associated with another disorder, such as multiple sclerosis or other disorders characterized by damage to the myelin sheath that covers certain nerves.
Is there any treatment?
Because there are a large number of conditions that can cause facial pain, TN can be difficult to diagnose. But finding the cause of the pain is important as the treatments for different types of pain may differ. Treatment options include medicines such as anticonvulsants and tricyclic antidepressants, surgery, and complementary approaches. Typical analgesics and opioids are not usually helpful in treating the sharp, recurring pain caused by TN. If medication fails to relieve pain or produces intolerable side effects such as excess fatigue, surgical treatment may be recommended. Several neurosurgical procedures are available. Some are done on an outpatient basis, while others are more complex and require hospitalization. Some patients choose to manage TN using complementary techniques, usually in combination with drug treatment. These techniques include acupuncture, biofeedback, vitamin therapy, nutritional therapy, and electrical stimulation of the nerves.
What is the prognosis?
The disorder is characterized by recurrences and remissions, and successive recurrences may incapacitate the patient. Due to the intensity of the pain, even the fear of an impending attack may prevent activity. Trigeminal neuralgia is not fatal.
National Institutes of Health (NHI.gov)
Pain Relief Self Advocacy
The APC Physicians encourage you to use the APCNoPain.com Patient Center Pain Pages and the following National Institures of Health Websites to assist in your quest for Chronic Pain Relief and a Healthier, Fuller Life.
• NIH.gov • National Institutes of Health (NIH)
• NLM.NIH.gov • U.S. National Library of Medicine
• Salud.NIH.gov Español • National Institutes of Health (NIH)
• NIH.gov/institutes-nih • NIH Institutes
• NIHPublications.OD.NIH.gov • NIH Publications Search Engine
NIH Sources for this Website
National Institutes of Health (NIH) • 9000 Rockville Pike, Bethesda, MD 20892
• NINDS.NIH.gov • NIH – National Institute of Neurological Disorders and Stroke
• NIAMS.NIH.gov • NIH – National Institute of Arthritis and Musculoskeletal and Skin Diseases
• NCCIH.NIH.gov • NIH – National Center for Complementary and Integrative Health
• Cancer.gov • NIH – National Cancer Institute
All NIH prepared information is in the Public Domain and may be freely reproduced and distributed.
Disclaimer
The information on this website is designed to support, not replace, the relationship between a site visitor / patient and his/her physician. If you have a medical emergency, call 911. For additional detail click this link: Terms of Use.
A common example of Referred Pain would be Knee Pain that originates from areas of the body besides the knee joint itself. These “referring areas” could be the Spine or Nerves, Knee Muscles, or Knee Tendons.
Spine & Nerves
Spine & Nerves – as Referring Source of Knee Pain
- Nerves are Infamous for “Referring Pain Elsewhere”.
- The Saphenous Nerve exits through the Adductor Muscle and if trapped can cause pain inside the knee that can travel down the inside of the leg to the ankle.
- The Tibial Nerve at the back of the knee can get compressed by a Baker’s Cyst leading to numbness, tingling and/or burning feelings radiating down the leg.
- Bulging Spinal Discs (tissue between the spine’s vertebrae) can pinch nerves that can make the knee area hurt or cause burning, tingling, numbness, or tightness in certain muscles. The S1 Nerve can cause symptoms in the back of the knee while the upper Lumbar Nerves can cause symptoms in the front of the knee or thigh.
Muscles
Muscles – as Referring Source of Knee Pain
- Muscles can develop “Trigger Points”, aka “Muscle Knots”, which are muscle areas that are painful and weak, and when pressed often “Refer Pain” to other parts of the body.
- Low Back Muscles (often L1-L3) can develop Trigger Points that refer pain to the knee.
- Quadriceps Muscle Trigger Points can refer pain to the knee.
Tendons
Tendons – as Referring Source of Knee Pain
- Tendons are the Fibrous Ends of the Muscles; they attach muscles to bones.
- Knee Tendons can become chronically tender and swollen.
- The Pes Anserine is the “Tennis Elbow” of the knee, located just below the inside of the knee where three important thigh muscles attach. Chronic back pain often make the Pes Anserine tender and swollen.
- The Patellar Tendon at the end of the quadriceps muscle contains the knee cap and when overloaded through trigger points, muscular weakness or excessive trauma, becomes chronically swollen and sore.
Knee Joint
Knee Joint – as Source
- Meniscus Tears or Arthritis in the Knee cause knee pain.
- The knee meniscus is “Shock Absorbing” spacer tissue; when torn, it can cause swelling or knee locking.
- The Knee Joint Cartilage can be worn away or torn through trauma, leading to arthritis.
- The Knee’s ACL is a major stabilizer of the front-back motion of the two knee bones.
- Excessive motion when the ACL is torn or stretched can lead to swelling, meniscus damage or arthritis.
- The MCL and LCL “Collateral Ligaments” are the “Duct Tape” that holds the sides of the knee together.
- A stretched or torn MCL or LCL can lead to excess movement that can cause damage to the inside knee structures.
Click to download NIH brochure: Peripheral Neuropathy
Peripheral Neuropathy – Contents
- What is peripheral neuropathy?
- How are the peripheral neuropathies classified?
- What are the symptoms of peripheral nerve damage?
- What causes peripheral neuropathy?
- How is peripheral neuropathy diagnosed?
- What treatments are available?
- What research is being done?
- Where can I get more information?
Pain Relief Self Advocacy
The APC Physicians encourage you to use the APCNoPain.com Patient Center Pain Pages and the following National Institures of Health Websites to assist in your quest for Chronic Pain Relief and a Healthier, Fuller Life.
• NIH.gov • National Institutes of Health (NIH)
• NLM.NIH.gov • U.S. National Library of Medicine
• Salud.NIH.gov Español • National Institutes of Health (NIH)
• NIH.gov/institutes-nih • NIH Institutes
• NIHPublications.OD.NIH.gov • NIH Publications Search Engine
National Institutes of Health – content sources used with permission for this website
National Institutes of Health (NIH) • 9000 Rockville Pike, Bethesda, MD 20892
• NINDS.NIH.gov • NIH – National Institute of Neurological Disorders and Stroke
• NIAMS.NIH.gov • NIH – National Institute of Arthritis and Musculoskeletal and Skin Diseases
• NCCIH.NIH.gov • NIH – National Center for Complementary and Integrative Health
• Cancer.gov • NIH – National Cancer Institute
All NIH prepared information is in the Public Domain and may be freely reproduced and distributed.
Disclaimer
The information on this website is designed to support, not replace, the relationship between a site visitor / patient and his/her physician. If you have a medical emergency, call 911. For additional detail click this link: Terms of Use.
Joint Conditions
Bursitis of the Hip (Trochanteric Bursitis)
Complex Regional Pain Syndrome (CRPS)
Lumbar Radiculopathy (Sciatica)
Peripheral Neuropathy
Piriformis Syndrome
Plantar Fasciitis
APC Joint Treatments