National Cancer Institute
at the National Institutes of Health (NHI – NCI)
General Information About Cancer Pain
Key Points
- Cancer, treatment for cancer, or diagnostic tests may cause you to feel pain.
- Pain control can improve your quality of life.
- Pain can be managed before, during, and after diagnostic and treatment procedures.
- Different cancer treatments may cause specific types of pain.
- Cancer pain may affect quality of life and ability to function even after treatment ends.
- Each patient needs a personal plan to control cancer pain.
- Cancer, treatment for cancer, or diagnostic tests may cause you to feel pain.
Pain is one of the most common symptoms in cancer patients. Pain can be caused by cancer, treatment for cancer, or a combination of factors. Tumors, surgery, intravenous chemotherapy, radiation therapy, targeted therapy, supportive care therapies such as bisphosphonates, and/or diagnostic procedures may cause you pain.
Younger patients are more likely to have cancer pain and pain flares than older patients. Patients with advanced cancer have more severe pain, and many cancer survivors have pain that continues after cancer treatment ends.
Pain control can improve your quality of life.
Pain can be controlled in most patients with cancer. Although cancer pain cannot always be relieved completely, there are ways to lessen pain in most patients. Pain control can improve your quality of life all through your cancer treatment and after it ends.
Pain can be managed before, during, and after diagnostic and treatment procedures.
Many diagnostic and treatment procedures are painful. It helps to start pain control before the procedure begins. Some drugs may be used to help you feel calm or fall asleep. Treatments such as imagery or relaxation can also help control pain and anxiety related to treatment. Knowing what will happen during the procedure and having a relative or friend stay with you may also help lower anxiety.
Different cancer treatments may cause specific types of pain.
Patients may have different types of pain depending on the treatments they receive, including:
- Spasms, stinging, and itching caused by intravenous chemotherapy.
- Mucositis (sores or inflammation in the mouth or other parts of the digestive system) caused by chemotherapy or targeted therapy.
- Skin pain, rash, or hand-foot syndrome (redness, tingling, or burning in the palms of the hands and/or the soles of feet) caused by chemotherapy or targeted therapy.
- Pain in joints and muscles throughout the body caused by paclitaxel or aromatase inhibitor therapy.
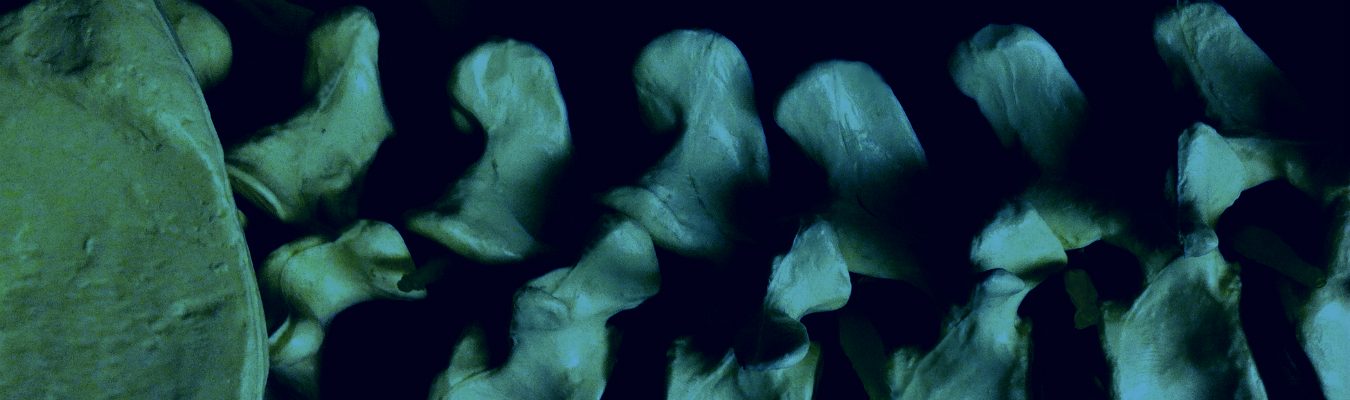
- Osteonecrosis of the jaw caused by bisphosphonates given for cancer that has spread to the bone.
- Pain syndromes, including mucositis, inflammation in areas receiving radiation therapy, pain flares, and dermatitis, caused by radiation.
- Cancer pain may affect quality of life and ability to function even after treatment ends.
Pain that is severe or continues after cancer treatment ends increases the risk of anxiety and depression. Patients may be disabled by their pain, unable to work, or feel that they are losing support once their care moves from their oncology team back to their primary care team. Feelings of anxiety and depression can worsen cancer pain and make it harder to control.
Each patient needs a Personal Plan to control cancer pain.
Each person’s diagnosis, cancer stage, response to pain, and personal likes and dislikes are different. For this reason, each patient needs a personal plan to control cancer pain. You, your family, and your healthcare team can work together to manage your pain. As part of your pain control plan, your healthcare provider can give you and your family members written instructions to control your pain at home. Find out who you should call if you have questions.
Assessment of Cancer Pain
Key Points
- You and your healthcare team work together to assess cancer pain.
- Physical and neurological exams will be done to help plan pain control.
You and your healthcare team work together to assess cancer pain.
It’s important that the cause of the pain is found early and treated quickly. Your healthcare team will help you measure pain levels often, including at the following times:
- After starting cancer treatment.
- When there is new pain.
- After starting any type of pain treatment.
To learn about your pain, the healthcare team will ask you to describe the pain with the following questions:
- When did the pain start?
- How long does the pain last?
- Where is the pain? You will be asked to show exactly where the pain is on your body or on a drawing of a body.
- How strong is the pain?
- Have there been changes in where or when the pain occurs?
- What makes the pain better or worse?
- Is the pain worse during certain times of the day or night?
- Is there breakthrough pain (intense pain that flares up rapidly even when pain-control medicine is being used)?
- Do you have symptoms, such as trouble sleeping, fatigue, depression, or anxiety?
- Does pain get in the way of activities of daily life, such as eating, bathing, or moving around?
Your healthcare team will also take into account:
- Past and current pain treatments.
- Prognosis (chance of recovery).
- Other conditions you may have, such as kidney, liver, or heart disease.
- Past and current use of nicotine, alcohol, or sleeping pills.
- Personal or family history of substance abuse.
- Personal history of childhood sexual abuse.
- Your own choices.
This information will be used to decide how to help relieve your pain. This may include drugs or other treatments. In some cases, patients are referred to pain specialists or palliative care specialists. Your healthcare team will work with you to decide whether the benefits of treatment outweigh any risks and how much improvement you should expect. After pain control is started, the doctor will continue to assess how well it is working for you and make changes if needed.
A family member or caregiver may be asked to give answers for a patient who has a problem with speech, language, or understanding.
Physical and neurological exams will be done to help plan pain control.
The following exams will be done:
Physical Exam and History: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of your health habits and past illnesses and treatments will also be taken.
Neurological Exam: A series of questions and tests to check the brain, spinal cord, and nerve function. The exam checks your mental status, coordination, and ability to walk normally, and how well the muscles, senses, and reflexes work. This may also be called a neuro exam or a neurologic exam.
Your healthcare team will also assess your psychological, social, and spiritual needs.
Using Drugs to Control Cancer Pain
Key Points
- The doctor will prescribe drugs based on whether the pain is mild, moderate, or severe.
- Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to relieve mild pain.
- Opioids are used to relieve moderate to severe pain.
- Most patients with cancer pain will need to receive opioids on a regular schedule.
- Opioids may be given in different ways.
- Common side effects are constipation, nausea, and drowsiness.
- Other drugs may be added to help treat your pain.
The doctor will prescribe drugs based on whether the pain is mild, moderate, or severe.
Your doctor will prescribe drugs to help relieve your pain. These drugs need to be taken at scheduled times to keep a constant level of the drug in the body to help keep the pain from coming back. Drugs may be taken by mouth or given in other ways, such as by infusion or injection.
Your doctor may prescribe extra doses of a drug that can be taken as needed for pain that occurs between scheduled doses of the drug. The doctor will adjust the drug dose for your needs.
A scale from 0 to 10 is used to measure how severe the pain is and decide which pain medicine to use. On this scale:
- 0 means no pain.
- 1 to 3 means mild pain.
- 4 to 6 means moderate pain.
- 7 to 10 means severe pain.
Acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to relieve mild pain.
Acetaminophen and NSAIDs help relieve mild pain. They may be given with opioids for moderate to severe pain.
Pain relievers of this type include:
- Acetaminophen
- Celecoxib
- Diclofenac
- Ibuprofen
- Ketoprofen
- Ketorolac
Patients, especially older patients, who are taking acetaminophen or NSAIDs need to be closely watched for side effects. See Treating Cancer Pain in Older Patients for more information.
Opioids are used to relieve moderate to severe pain.
Opioids work very well to relieve moderate to severe pain. Some patients with cancer pain stop getting pain relief from opioids if they take them for a long time. This is called tolerance. Larger doses or a different opioid may be needed if your body stops responding to the same dose. Tolerance of an opioid is a physical dependence on it. This is not the same as addiction (psychological dependence). Opioid doses can be safely increased by your doctor as needed for your pain, without causing addiction.
There are several types of opioids:
- Buprenorphine
- Codeine
- Diamorphine
- Fentanyl
- Hydrocodone
- Hydromorphone
- Methadone
- Morphine (the most commonly used opioid for cancer pain)
- Oxycodone
- Oxymorphone
- Tapentadol
- Tramadol
The doctor will prescribe drugs and the times they should be taken in order to best control your pain. Also, it is important that patients and family caregivers know how to safely use, store, and dispose of opioids.
Most patients with cancer pain will need to receive opioids on a regular schedule.
Receiving opioids on a regular schedule helps control the pain and keeps it from getting worse. The amount of time between doses depends on which opioid is being used. The correct dose is the amount of opioid that controls your pain with the fewest side effects. The dose will be slowly adjusted until there is a good balance between pain relief and side effects. If opioid tolerance does occur, the dose may be increased or a different opioid may be needed.
Opioids may be given in different ways.
Opioids may be given by the following ways:
Mouth: If your stomach and intestines work normally, medicine is usually given by mouth. Opioids given orally are easy to use and usually low-cost. Oral opioids are sometimes placed under the tongue (sublingual route) or on the inside of the cheek (buccal route) to be absorbed.
Rectum: If you cannot take opioids by mouth, they may be given as rectal suppositories.
Skin patches: Opioid patches are placed on the skin (transdermal route).
Nose spray: Opioids may be given in the form of a nasal spray.
Intravenous (IV) line: Opioids are given into a vein only when simpler and less costly methods cannot be used, don’t work, or are not wanted by the patient. Patient-controlled analgesia (PCA) pumps are one way to control pain through your IV line. A PCA pump allows you to control the amount of drug that is used. With a PCA pump, you can receive a preset opioid dose by pressing a button on a computerized pump that is connected to a small tube. Once the pain is controlled, the doctor may prescribe regular opioid doses based on the amount you used with the PCA pump.
Subcutaneous injection: Opioids are given by injection into the fatty layer of tissue just under the skin.
Intraspinal injection: Intraspinal opioids are injected into the fluid around the spinal cord. These may be combined with a local anesthetic to help some patients who have pain that is very hard to control.
Common side effects are constipation, nausea, and drowsiness.
Your doctor will discuss the side effects with you before opioid treatment begins and will watch you for side effects. The following are the most common side effects:
- Constipation
- Nausea
- Drowsiness
- Dry mouth
Drowsiness and nausea most often occur when opioid treatment is first started and usually get better within a few days.
Opioids slow down the muscle contractions and movement in the stomach and intestines, which can cause hard stools. To keep the stool soft and prevent constipation, it’s important to drink plenty of fluids. Unless there are problems such as a blocked bowel or diarrhea, you will be given a treatment plan to follow to prevent constipation and information on how to avoid problems with your intestines while taking opioids.
Other side effects of opioid treatment include the following:
- Vomiting
- Low blood pressure
- Dizziness
- Trouble sleeping
- Trouble thinking clearly
- Delirium or hallucinations
- Trouble urinating
- Problems with breathing
- Severe itching
- Problems with sexual function
- Hot flashes
- Depression
- Hypoglycemia
Talk with your doctor about side effects that bother you or become severe. Your doctor may decrease the dose of the opioid, change to a different opioid, or change the way the opioid is given to help decrease the side effects. See the following PDQ summaries for more information about coping with these side effects:
- Gastrointestinal Complications
- Nausea and Vomiting
- Delirium
Other drugs may be added to help treat your pain.
Other drugs may be given while you are taking opioids for pain relief. These are drugs that help the opioids work better, treat symptoms, and relieve certain types of pain. The following types of drugs may be used:
- Antidepressants
- Anticonvulsants
- Local anesthetics
- Corticosteroids
- Stimulants
- Bisphosphonates and denosumab
There are big differences in how patients respond to these drugs. Side effects are common and should be reported to your doctor.
Bisphosphonates (pamidronate and zoledronic acid) are drugs that are sometimes used when cancer has spread to the bones. They are given as an intravenous infusion and combined with other treatments to decrease pain and reduce risk of broken bones. However, bisphosphonates sometime cause severe side effects. Talk to your doctor if you have severe muscle or bone pain. Bisphosphonate therapy may need to be stopped.
The use of bisphosphonates is also linked to the risk of bisphosphonate-associated osteonecrosis (BON). See the PDQ summary on Oral Complications of Chemotherapy and Head/Neck Radiation for more information.
Denosumab is another type of drug therapy that may be used when cancer has spread to the bones. It is given as a subcutaneous injection and may help prevent and relieve pain. It is not used in certain patients, such as patients with myeloma.
Other Treatments for Cancer Pain
Key Points
- Nerve blocks
- Neurological treatments
- Cordotomy
- Palliative care
- Radiation therapy
- External radiation therapy
- Radiopharmaceuticals
- Physical medicine and rehabilitation
Complementary Therapies
- Acupuncture
- Hypnosis
- Support groups
Most cancer pain can be controlled with drug treatments, but some patients have too many side effects from drugs or have pain in a certain part of the body that needs to be treated in a different way. You can talk to your doctor to help decide which methods work best to relieve your pain. These other treatments include:
Nerve Blocks
A nerve block is the injection of either a local anesthetic or a drug into or around a nerve to block pain. Nerve blocks help control pain that can’t be controlled in other ways. Nerve blocks may also be used to find where the pain is coming from, to predict how the pain will respond to long-term treatments, and to prevent pain after certain procedures.
Neurological Treatments
Surgery can be done to insert a device that delivers drugs or stimulates the nerves with mild electric current. In rare cases, surgery may be done to destroy a nerve or nerves that are part of the pain pathway.
Cordotomy
Cordotomy is a less common surgical procedure that is used to relieve pain by cutting certain nerves in the spinal cord. This blocks pain and also hot/cold feelings. This procedure may be chosen for patients who are near the end of life and have severe pain that cannot be relieved in other ways.
Palliative Care
Certain patients are helped by palliative care services. Palliative care providers may also be called supportive care providers. They work in teams that include doctors, nurses, mental health specialists, social workers, chaplains, pharmacists, and dietitians. Some of the goals of palliative care are to:
- Improve quality of life for patients and their families.
- Manage pain and non-pain symptoms.
- Support patients who need higher doses of opioids, have a history of substance abuse, or are coping with emotional and social problems.
Radiation Therapy
Radiation therapy is used to relieve pain in patients with skin lesions, other tumors, or cancer that has spread to the bone. This is called palliative radiation therapy. It may be given as local therapy directly to the tumor or to larger areas of the body. Radiation therapy helps drugs and other treatments work better by shrinking tumors that are causing pain. Radiation therapy may help patients with bone pain move more freely and with less pain.
The following types of radiation therapy may be used:
External Radiation Therapy
External radiation therapy uses a machine outside the body to send high-energy x-rays or other types of radiation aimed toward the cancer. External radiation therapy relieves pain from cancer that has spread to the bone. Radiation therapy may be given in a single dose or divided into several smaller doses given over a period of time. The decision whether to have single or divided dose may depend on how easy it is to get the treatments and how much they cost.
Radiopharmaceuticals
Radiopharmaceuticals are drugs that have a radioactive substance that may be used to diagnose or treat disease, including cancer. Radiopharmaceuticals may also be used to relieve pain from cancer that has spread to the bone. A single dose of a radioactive agent injected into a vein may relieve pain when cancer has spread to several areas of bone and/or when there are too many areas to treat with external radiation therapy.
Physical Medicine and Rehabilitation
Patients with cancer and pain may lose their strength, freedom of movement, and ability to manage their daily activities. Physical therapy or occupational therapy may help these patients.
Physical medicine uses physical methods, such as exercise and machines to prevent and treat disease or injury.
Physical methods to treat weakness, muscle wasting, and muscle and bone pain include the following:
- Exercise to strengthen and stretch weak muscles, loosen stiff joints, help coordination and balance, and strengthen the heart.
- Changing position (for patients who are not able to move on their own).
- Limiting the movement of painful areas or broken bones.
Some patients may be referred to a physiatrist (a doctor who specializes in physical medicine) who can develop a personal plan for them. Some physiatrists are also trained in procedures to treat and manage pain.
Complementary Therapies
Complementary and alternative therapies combined with standard treatment may be used to treat pain. They may also be called integrative therapies. Acupuncture, support groups, and hypnosis are a few integrative therapies that have been used to relieve pain.
Acupuncture
Acupuncture is an integrative therapy that applies needles, heat, pressure, and other treatments to one or more places on the skin called acupuncture points. Acupuncture may be used to control pain, including pain related to cancer. See the PDQ summary on Acupuncture for more information.
Hypnosis
Hypnosis may help you relax and may be combined with other thinking and behavior methods. Hypnosis to relieve pain works best in people who are able to concentrate and use imagery and who are willing to practice the technique.
Support groups
Support groups help many patients. Religious counseling may also help by offering spiritual care and social support.
Complementary and Alternative Medicine (CAM) for Cancer Pain
Complementary and alternative medicine (CAM) is the term for medical products and practices that are not part of standard medical care.
Standard medical care is medicine that is practiced by health professionals who hold an M.D. (medical doctor) or D.O. (doctor of osteopathy) degree. It is also practiced by other health professionals, such as physical therapists, physician assistants, psychologists, and registered nurses. Standard medicine may also be called biomedicine or allopathic, Western, mainstream, orthodox, or regular medicine. Some standard medical care practitioners are also practitioners of CAM.
Complementary medicine is treatments that are used along with standard medical treatments but are not considered to be standard treatments. One example is using acupuncture to help lessen some side effects of cancer treatment.
Alternative medicine is treatments that are used instead of standard medical treatments. One example is using a special diet to treat cancer instead of anticancer drugs that are prescribed by an oncologist.
Integrative medicine is a total approach to medical care that combines standard medicine with the CAM practices that have shown to be safe and effective. They treat the patient’s mind, body, and spirit.
NCI provides evidence-based PDQ information for many CAM therapies in versions for both the patient and health professional.
Are CAM Approaches Safe?
Some CAM therapies have undergone careful evaluation and have found to be safe and effective. However there are others that have been found to be ineffective or possibly harmful. Less is known about many CAM therapies, and research has been slower for a number of reasons:
Regulatory Issues
CAM therapies need to be evaluated with the same long and careful research process used to evaluate standard treatments. Standard cancer treatments have generally been studied for safety and effectiveness through an intense scientific process that includes clinical trials with large numbers of patients.
Natural Does Not Mean Safe
CAM therapies include a wide variety of botanicals and nutritional products, such as dietary supplements, herbal supplements, and vitamins. Many of these “natural” products are considered to be safe because they are present in, or produced by, nature. However, that is not true in all cases. In addition, some may affect how well other medicines work in your body. For example, the herb St. John’s wort, which some people use for depression, may cause certain anticancer drugs not to work as well as they should.
Herbal supplements may be harmful when taken by themselves, with other substances, or in large doses. For example, some studies have shown that kava kava, an herb that has been used to help with stress and anxiety, may cause liver damage.
Vitamins can also have unwanted effects in your body. For example, some studies show that high doses of vitamins, even vitamin C, may affect how chemotherapy and radiation work. Too much of any vitamin is not safe, even in a healthy person.
Tell your doctor if you’re taking any dietary supplements, no matter how safe you think they are. This is very important. Even though there may be ads or claims that something has been used for years, they do not prove that it’s safe or effective.
Supplements do not have to be approved by the federal government before being sold to the public. Also, a prescription is not needed to buy them. Therefore, it’s up to consumers to decide what is best for them.
NCI and the National Center for Complementary and Integrative Health (NCCIH) are currently sponsoring or cosponsoring various clinical trials that test CAM treatments and therapies in people. Some study the effects of complementary approaches used in addition to conventional treatments, and some compare alternative therapies with conventional treatments. Find all cancer CAM clinical trials.
What Should Patients Do When Using or Considering CAM Therapies?
Cancer patients who are using or considering using complementary or alternative therapy should talk with their doctor or nurse. Some therapies may interfere with standard treatment or even be harmful. It is also a good idea to learn whether the therapy has been proven to do what it claims to do.
To find a CAM practitioner, ask your doctor or nurse to suggest someone. Or ask if someone at your cancer center, such as a social worker or physical therapist can help you. Choosing a CAM practitioner should be done with as much care as choosing a primary care provider.
Patients, their families, and their health care providers can learn about CAM therapies and practitioners from the following government agencies:
National Center for Complementary and Integrative Health
NCI Office of Cancer Complementary and Alternative Medicine
Office of Dietary Supplements
Updated: April 10, 2015
Treating Cancer Pain in Older Patients
Key Points
Older patients with cancer pain may have special needs.
- Lower doses
- More than one chronic disease and source of pain
- Side effects of nonsteroidal anti-inflammatory drugs (NSAIDs)
- Effects of opioids
- Patient-controlled pain relief
- Changes in living arrangements
Older Patients with Cancer Pain may have Special Needs.
Some problems are more likely in older patients. For caregivers of older patients, the following should be kept in mind:
Lower Doses
Pain medicine should be started at lower doses in older patients and adjusted slowly to allow for differences in their pain threshold and the ways they respond and function.
Older patients may need simpler and more frequent tests to find out how much pain they are having.
More than one Chronic Disease and Source of Pain
Older patients may have more than one chronic disease and take several drugs for different conditions. This can increase the risk of drug interactions. Drugs taken together can change how they work in the body and can affect the patient’s chronic diseases.
Side effects of nonsteroidal anti-inflammatory drugs (NSAIDs)
Side effects of NSAIDs, such as stomach and kidney damage, memory problems, constipation, and headaches, are more likely in older patients.
NSAIDS and tricyclic antidepressants are not to be given to certain older patients.
Effects of Opioids
Older patients may need lower doses of opioids since they are more sensitive to their effects. Lower doses of opioids may give older patients better pain relief that lasts longer than in younger patients.
Opioid doses may need to be adjusted lower when treating older patients for either acute or chronic pain and when given by mouth, injection, or other ways.
Patient-controlled Pain Relief
Patient-controlled pain relief must be used carefully in older patients, since drugs are slower to leave the body and older patients are more sensitive to the side effects.
Changes in Living Arrangements
When older patients move (for example, from hospital to home or nursing home), their needs for pain control may change. These needs should be checked so that pain control methods can be adjusted if needed.
- Pain is often a harsh reality of cancer, and can be caused either by the cancer tumor or by the radiation, chemotherapy or surgical cancer treatments.
- 80% – 85% of cancer patients’ pain can be significantly relieved.
- The remaining 15% – 20% of patients have cancer pain that is difficult to manage.
- 80% of advanced-stage cancer patients have moderate to severe cancer pain.
- Cancer patients are disabled an average of 12 to 20 days per month.
- With 28% to 55% unable to work because of their cancer.
- In 68% of patients the chief cause of cancer pain is the primary tumor.
- The other 32% of patients experience pain from the cancer treatments and procedures.
- Sources: Cancer.gov & NIH.gov
National Cancer Institute
at the National Institutes of Health (NHI – NCI)
Thinking About Complementary and Alternative Medicine
Thinking About Complementary and Alternative Medicine is for people who want to try additional methods to help them cope with side effects during cancer treatment, or to deal with stress and other discomforts.
Click to Download Booklet: CAM for Cancer Pain
This booklet covers:
- What complementary and alternative medicine is (CAM) is and why people use it
- The different types of CAM (mind-body methods, biologically based practices, body-based practices, energy medicine, and whole medical systems.
- How to talk to your doctor about CAM and the questions to ask
- A natural product isn’t always a safe product
- How to choose a CAM specialist and questions to ask
- Getting information from trusted resources such as government agencies and websites
Support for People with Cancer Pain
Pain Control is for people who have pain from cancer or from its treatment. Family and friends may also want to read this booklet.
Having cancer doesn’t mean you’ll have pain. But if you do, this booklet includes tips about managing your pain with medicine and other treatments.
Click to Download Booklet: Support People with Cancer Pain
This booklet covers:
- The types and causes of cancer pain
- How to talk about your pain with your health care team
- How to make your pain control plan work for you
- Pain control medicines and side effects
- Medicine tolerance is not addiction
- Other ways to control pain
- How having pain can affect your thoughts and feelings
- Financial issues and paying for pain medicine
- Cancer pain can almost always be relieved. Talk with your doctor and health care team about any pain you are having.
The information in this booklet was last updated in May 2014.
National Cancer Institute
at the National Institutes of Health (NHI – NCI)
Pain Relief Self Advocacy
The APC Physicians encourage you to use the APCNoPain.com Patient Center Pain Pages and the following National Institures of Health Websites to assist in your quest for Chronic Pain Relief and a Healthier, Fuller Life.
• NIH.gov • National Institutes of Health (NIH)
• NLM.NIH.gov • U.S. National Library of Medicine
• Salud.NIH.gov Español • National Institutes of Health (NIH)
• NIH.gov/institutes-nih • NIH Institutes
• NIHPublications.OD.NIH.gov • NIH Publications Search Engine
NIH Sources for this Website
National Institutes of Health (NIH) • 9000 Rockville Pike, Bethesda, MD 20892
• NINDS.NIH.gov • NIH – National Institute of Neurological Disorders and Stroke
• NIAMS.NIH.gov • NIH – National Institute of Arthritis and Musculoskeletal and Skin Diseases
• NCCIH.NIH.gov • NIH – National Center for Complementary and Integrative Health
• Cancer.gov • NIH – National Cancer Institute
All NIH prepared information is in the Public Domain and may be freely reproduced and distributed.
Disclaimer
The information on this website is designed to support, not replace, the relationship between a site visitor / patient and his/her physician. If you have a medical emergency, call 911. For additional detail click this link: Terms of Use.
Complementary and Alternative Medicine for Cancer Pain (0:1:48)
Dr. Jeffrey D. White, OCCAM Director, explains the use of complementary and alternative medicine in cancer.

